Information for patients
This leaflet can be made available in other formats including large print, CD and Braille and in languages other than English, upon request.
Introduction
This leaflet aims to give you information about a procedure called Endoscopic Ultrasound (EUS) Guided Gallbladder Drainage and what it involves.
This is a new way doctors can treat patients who need gallbladder drainage. Before you decide, its important you understand why this procedure is being proposed and what it will involve. It is important that you are fully aware of the benefits and risks of this procedure before you sign the consent form.
Please read this leaflet carefully before coming for the procedure so that you can ask any questions you may have when you attend.
You will be asked to sign the consent form after you have had a chance to ask questions.
What is Endoscopic Ultrasound (EUS) Guided Gallbladder Drainage?
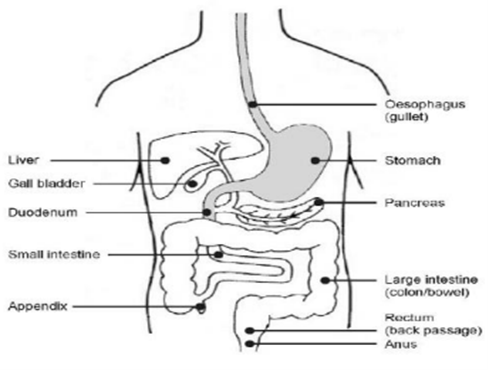
You have been advised to have an EUS. This is a procedure that allows an Endoscopist (a consultant trained to do EUS) to see inside of your oesophagus (gullet or food pipe), stomach and duodenum (small intestine) and the organs outside of it (liver, pancreas, gall bladder, kidneys, adrenal glands, lymph glands, blood vessels and nerves) using an EUS endoscope.
An EUS endoscope (a thin, flexible tube with a bright light and a small ultrasound probe on the end) will be passed through your mouth and down into your stomach and small bowel.
Once the EUS endoscope is in position, ultrasound waves are used to see the area and structures deeper in the chest and abdomen.
Your doctor has requested to carry out EUD as this will allow the gallbladder to be seen and guide the placement of the stent between the gallbladder and the stomach or the duodenum (beginning of the small bowel) to allow drainage of the gallbladder.
This will be explained to you in more detail before the procedure. You will need to have a blood test before the procedure to check that your blood is clotting properly.
What is cholecystitis?
The liver produces bile and the gallbladder acts as a reservoir for bile. It is common for stones to form within the gallbladder.
Sometimes, the bile in the gallbladder can become infected with build-up of pus, usually due to blockage with gallstones. In medical terms, this condition is called cholecystitis.
If your gallbladder is infected, you will be very unwell with fever and abdominal pain. You will be admitted to the hospital and treated with antibiotics.
Who is this procedure for?
This procedure is carried out to drain the gallbladder in unwell patients with symptoms of abdominal (tummy) pain, fever and sepsis that is not settling with antibiotics.
Why am I having this procedure?
Your doctor has referred you for this procedure because you have displayed some of the above symptoms and they have not been helped by the standard treatment.
If the antibiotics are not enough to settle the infection, there is a risk that the gallbladder can burst.
Hence your doctor has decided to drain your gallbladder.
Are there any other procedures that can be done instead?
The ideal treatment for cholecystitis is a keyhole surgery to remove the gallbladder. Often a patient is too unwell or has other medical problems that make an immediate operation unsafe.
Some patients are deemed unsuitable for surgery under general anaesthesia due to pre-existing medical conditions.
In the above situations, the treatment over the years has been to drain the gallbladder using a long plastic tube which is inserted into the gallbladder by piercing the skin between the ribs at the bottom of the right side of the chest.
This allows drainage of the infected gallbladder material. This tube stays in place for a few weeks and is then removed.
This procedure is called a percutaneous gallbladder drain (percutaneous cholecystostomy).
In recent years, studies have shown that EUS guided gallbladder drainage is a more effective treatment for cholecystitis than a percutaneous gallbladder drain as it is more comfortable and reduces the likelihood of complications. For example, this would prevent hospital admissions due to a blocked or dislodged drain.
The stent placed under EUS guidance can also be left in permanently in-situ if the surgeons decide not to remove the gallbladder on a later date.
If left in-situ long term, the stent can help reduce the risks of further gallbladder infections in future.
You do not have to have any procedures you do not want, but the doctor who has requested the treatment has recommended this as being the best option for you.
What are the risks and possible complications?
Like all procedures, EUS guided gallbladder drainage procedure has some side effects or complications.
These include:
What will happen before my procedure?
You will be admitted to the Endoscopy Unit at North Tees on the morning of your procedure, unless you appointment letter states otherwise.
You will stay in hospital overnight so please be prepared for this. It might be useful to pack a bag with night clothes, toiletries and anything else that you think you may need.
Please do not bring anything valuable into hospital.
What will I need to do to prepare for my procedure?
It is very important you follow the instructions given into this leaflet to make sure your oesophagus (food pipe), stomach and duodenum (intestine and gut) are empty. This will allow the Endoscopist to get a clear view and make sure no areas are hidden.
You must stop eating or drinking at least 6 hours before your procedure. This is very important and you must follow the instructions, nothing means nothing at all.
If you forget and you do eat or drink anything, you must tell your Doctor or Nurse as your procedure may need to be delayed for your safety.
This is because when you are sedated, if your stomach contains food or drinks and you vomit (throw up), it could get into your lungs, affect your breathing and cause infection and/or other complications.
If you are taking any medication to thin your blood or if you are unsure, you must contact the Endoscopy Unit as soon as you get your appointment.
This medication includes anticoagulants such as Warfarin, Apixaban, Dabigatran, Rivaroxban amongst others, or antiplatelet medications such as Aspirin, Clopidogrel, Ticagrelor, Dipyridamole amongst others.
This will be discussed with you at your pre-assessment appointment.
You can continue to take Aspirin if you are already doing so, but you must stop taking this on the morning of your procedure.
If you have diabetes, you should contact the Endoscopy Unit for advice about your medication.
Can I be sedated for the procedure?
The procedure is usually carried out using conscious sedation.
Sometimes the procedure is carried out using deep sedation with the help of an anaesthetist. The effect on sedation will stay with you for at least 24 hours so it is important that you follow this advice.
This is because the effects of the sedation will affect your judgement.
For the first 24 hours after sedation:
- You must not go back to work.
- You must not drive a car, ride a bicycle or motorcycle. It is an offence to drive while unfit to do so because of drugs and it will likely invalidate your insurance policy.
- You must not supervise children.
- You must not make important decisions or sign any legal documents.
- You must not operate machinery or electrical appliances.
- You must not go near open flames or sources of high heat.
- You must not drink alcohol.
- You must not take sleeping tablets, tranquilisers or any drugs other than those prescribed for you by your GP.
- You must not lock the toilet or bathroom door in case you need any help.
- You must not smoke.
What will happen when I arrive for my appointment?
When you arrive at the Endoscopy Unit, you will be advised by the Endoscopy Nurse of an approximate time you should be ready to go home.
There is limited space in the unit, so only in special cases will someone be allowed to stay with you, for example, adults with special needs.
A Nurse will call you through to the unit. They will check your personal details and ask you to a few questions about your health.
They will also check your blood pressure and pulse, explain the procedure and risks to you. This is to make sure you understand everything before you sign the consent form.
You should tell the Nurse if you have had any allergies or reaction to drugs or other procedures in the past. You should also tell your Nurse about any previous endoscopy procedures you may have had.
Please bring with you a list of medications (drugs) you are currently taking. This includes medicines prescribed by your Doctor or those you have brought for yourself.
Although it is likely you will be staying in the hospital after the procedure, you will still be asked for a contact telephone number of the relative or friend who will take you home and stay with you on discharge.
You will be taken to a comfortable waiting area to wait your turn. We operate a list system. This means you will be seen when it is your turn and not the time given for you to arrive at the unit.
Before your examination, if you have any worries or questions, please talk to your Nurse or Endoscopist.
What should I do on the day of my procedure?
On the day of your procedure, it is important that:
- You should not smoke.
- Long hair should be tied back for comfort.
- You avoid bringing valuables with you.
- You wear loose fitting clothing.
- False teeth, glasses and hearing aids may be removed in the Endoscopy room.
When it is time for your procedure, a Nurse will take you into the examination room.
What will happen during my procedure?
Before your procedure begins, you will be asked to remove any false teeth, if you have them. A local anaesthetic will be sprayed on to the back of your throat to numb the area.
You will be given a sedative drug before the examination starts. This is called conscious sedation. You will still be awake but should feel more comfortable and relaxed.
This involves injecting medication through a cannula (a fine tube) inserted into a vein in the back of your hand or arm using a small fine needle.
In the examination room, you will then be asked to lie down on a trolley on your left side. Your pulse, blood pressure and oxygen levels in your blood will be checked before and during your procedure.
A Nurse will make sure you are comfortable and your privacy and dignity will be maintained at all times through the procedure.
You will be given extra oxygen to breathe through a soft plastic tube that goes into your nose. a small plastic guard will be put gently between your teeth to protect them. Do not worry, this is all routine and is not painful.
The Endoscopist will then pass the EUS scope (camera) through your mouth into your stomach and then into your duodenum (gut). Air will be passed through the tube to inflate your stomach so that your Endoscopist can see all parts of your stomach and the small bowel wall.
This can cause “windy” discomfort. Using ultrasound guidance, a special type of stent (a lumen-apposing metal stent) is placed into your gallbladder through the wall of either your stomach duodenum.
The lumen-apposing metal stent creates an opening between the gallbladder and the stomach or duodenum. This allows the pus and infected bile to flow out of your gallbladder and into the bowel, which should usually lead to a rapid improvement in the infection and pain. You will continue to be treated with antibiotics.
During the procedure, any extra saliva will be cleared from your mouth using a fine suction tube. When the procedure is over, the air and the EUS camera are removed quickly and easily.
We routinely take photographs or videos of your insides during this procedure. These are used to help in your investigations and treatment. The procedure may take up between 45 – 60 minutes to be completed.
What happens to the pictures taken during my procedure?
The pictures taken during your procedure will be kept as part of your healthcare record. These may sometimes be used anonymously for training or research. If hospital staff want to use any of your pictures for any other purposes, for example, in an article to be published (printed) in a professional magazine or book, they will ask for your permission first before this happens.
What will happen after the procedure?
You will be taken to the recovery area where you will be able to rest on a trolley until the immediate effects of the sedation have worn off.
You will be given some fluids through the intravenous cannula (drip) to prevent hypotension (low blood pressure).
You’ll usually have to stay in hospital overnight for observation.
Should I take any special precautions after the procedure?
You might feel slightly more under the weather for the first 24 – 48 hours after your procedure. We recommend that you get plenty of rest during this time.
Because of the sedation given for the procedure, you will not be able to drive or operate heavy machinery for the next 24 hours.
What follow up is planned after my procedure?
A copy of the report will go to your referring team who will continue to manage your symptoms.
When will I be told about the outcome of my procedure?
Before you leave the unit, your Nurse or Endoscopist will explain the outcome of your procedure to you. A copy of your report will be sent to your GP within 24 hours.
If you are an in-patient, the Doctor responsible for your care will discuss the outcome of the procedure with you on the ward.
If you need further advice, or have any problems, please contact the Unit where you are to have your examination.
University Hospital of North Tees Endoscopy Unit
Telephone: 01642 624387, Monday to Friday – 8am to 7pm, Saturday 8am to 2pm
If you start to experience any significant pain, please attend the Emergency Department
Emergency Department
Telephone: 01642 382899, 24 hours a day, 7 days a week
Further Information is available from:
NHS Choices
Telephone 111 (when it is less urgent than 999) Calls to this number are free from landlines and mobile phones.
Website: www.nhs.uk
References
- Adverse events associated with EUS and EUS-guided Procedures, Nauzer Forbes, Nayantara Coelho-Prabhu, Mohammad A. Al-Haddad et al, ASGE Standards of Practice Committee, Gastrointestinal Endoscopy Volume 95, No. 1, 2022
- Therapeutic Endoscopic Ultrasound: European Society of Gastrointestinal Endoscopy Guideline Endoscopy. 2022 Feb;54(2):185-205. doi: 10.1055/a-1717-1391. Epub 2021 Dec 22
- Endosonography-guided gallbladder drainage versus percutaneous cholecystostomy in very high-risk surgical patients with acute cholecystitis: an international randomised multicentre controlled superiority trial (DRAC 1) Chiu PWY, Ng EKW, Lau JYW. Gut. 2020 Jun;69(6):1085-1091. doi: 10.1136/gutjnl-2019-319996. Epub 2020 Mar 12
- Outcomes and limitations in EUS-guided gallbladder drainage. Endosc Ultrasound. 2019 Nov 28;8(Suppl 1):S40-S43. doi: 10.4103/eus.eus_49_19. eCollection 2019 Nov
- Endoscopic ultrasound guided gallbladder drainage in acute cholecystitis when surgery is not an option. NICE guidelines published 22.6.2023
Comments, concerns, compliments or complaints
Patient Experience Team (PET)
We are continually trying to improve the services we provide. We want to know what we’re doing well or if there’s anything which we can improve, that’s why the Patient Experience Team (PET) is here to help. Our Patient Experience Team is here to try to resolve your concerns as quickly as possible. The office is based on the ground floor at the University Hospital of North Tees if you wish to discuss concerns in person. If you would like to contact or request a copy of our PET leaflet, please contact:
Telephone: 01642 624719
Freephone: 0800 092 0084
Opening hours: Monday to Friday, 9:30am to 4:00pm
Email: [email protected]
Out of hours
Out of hours if you wish to speak to a senior member of Trust staff, please contact the hospital switchboard who will bleep the appropriate person.
Telephone: 01642 617617
Data protection and use of patient information
The Trust has developed Data Protection policies in accordance with Data Protection Legislation (UK General Data Protection Regulations and Data Protection Act 2018) and the Freedom of Information Act 2000. All of our staff respect these policies and confidentiality is adhered to at all times. If you require further information on how we process your information please see our Privacy Notices.
Telephone: 01642 383551
Email: [email protected]
Privacy NoticesLeaflet feedback
This leaflet has been produced in partnership with patients and carers. All patient leaflets are regularly reviewed, and any suggestions you have as to how it may be improved are extremely valuable. Please write to the Clinical Governance team, North Tees and Hartlepool NHS Foundation Trust, University Hospital of North Tees, TS19 8PE or:
Email: [email protected]
Leaflet reference: PIL1461
Date for Review: October 2026