On this page
- 1. Introduction
- 2. Complaint definitions
- 3. Complaints received by year by stage
- 4. Top four themes by stage (all sub subjects)
- 5. Response to the complainant provided within agreed timeframes
- 6. Outcome classification of Stage 3 complaints
- 7. Actions and improvements undertaken 2022 – 23
- 8. Proposals and continued improvement in 2023 – 24
- 9. Further contacts received following a stage 2 or 3 complaint response
- 10. The parliamentary and health service ombudsman (PHSO)
- 11. Patient satisfaction surveys
- 12. Overall compliment status
- 13. Overall friends and family test return rate
- Appendix A.
- PDF Document download
1. Introduction
Welcome to our Patient Experience and Involvement Annual Report. Through this report we will share some of the work that has been undertaken with our staff, patients and carers during 2022-2023 and provide detail in relation to service user feedback such as complaints, compliments, Friend and Family Test, patient surveys and patient stories.
We would like to thank everyone who has worked with us over the past year: the patients and their family members, carers and our volunteers who have shared their insights and challenges to our work, during their experience with the Trust. Work has commenced with our patients, public and people with lived experience (PPPLE) to support us to co-design, test and challenge our thinking and approach to patient experience.
One of our Trust strategic aims is to put our population first – ‘it starts with me’, to help us to create a culture where staff listen to the patient, carer and family needs, then use this valuable experience when developing services.
Our key objective for patient experience and involvement is to work with our patients, service users and partners to ‘Deliver patient care that is safe, effective and person-centred’ by:
- Maximising the things that go right, minimising the things that go wrong
- Delivering good outcomes, based on the best available evidence
- Care is shaped by what matters to people
This report is compiled on an annual basis for the Quality Assurance Committee (formally the Patient Safety & Quality Standards Committee) to provide assurance of patient engagement and that there is a robust complaint process in place within the Trust. Data is provided from the previous year as a comparison to identify any trends.
The report also identifies improvements the organisation made based upon the findings of a trend analysis of complaint data. Action taken as a result of the analysis of patient feedback can impact by improving the experience and service provided to our patients. The improvements identified support the prevention of further complaints regarding the same or similar issues.
The number of complaints received into the organisation together with trends is discussed during weekly Safety Panel Meetings, Senior Clinical Professional Huddles and Care Group meetings and actions identified as appropriate.
The Trust commenced a review of the complaint process in line with the Parliamentary Health Service Ombudsman (PHSO) Complaint Standards Framework towards the end of 2022. The Stage 3 revised process (written complaint response) had a go live date of 3 January 2023, and a work plan was developed to ensure all stages and associated processes will be fully reviewed and updated by the end of Quarter 2, 2023-2024.
External training opportunities were identified for key personnel in relation to responding to complaints, with an initial training session held in March 2023. Online training opportunities for all staff involved in complaints management were made available by the PHSO during Quarter 1, 2023-2024.
Engaging patients and understanding their experience
The Trust is on a journey of discovery in how we involve and engage patients, people and public in continuous improvement based on lived experiences.
The patient experience portfolio has developed significantly over the last few years supporting staff in understanding how we can collaborate, involve and work with patients, carers and service users in identifying opportunities to involve them in co-design and co-production of services to improve patient experience and patient safety.
Our patient experience and involvement priorities are to deliver patient-centred care – ‘it starts with me’:
Insight – By proactively seeking patient stories, compliments, friends and family test returns, and complaints and using data from local and national surveys to drive forward changes to improve patient experience.
Involve – By involving people at every stage.
Improve – By providing services that are accessible and inclusive for all through collaboration with key stakeholders.
Healthcare User Group
We have worked closely with our Healthcare User Group members who regularly attend a wide variety of Councils and Committees in the Trust. This provides the opportunity for service user involvement in decision making. The Group have continued to visit areas within the Trust to carry out assessments of the environment and speak with patients and staff to gain valuable feedback.
Improvements for 2023-2024 to support this valuable resource, will be to include enhancing and developing the Health Care User Group roles into Patient Experience Partner roles working within existing assessment streams such as PLACE and Appreciative Support visits.
Patient, People and Public with Lived Experience (PPPLE) Group
Inform:
Share information about proposed changes and service improvements so that people feel informed and are aware.
Goals:
Develop a process and proforma so that staff can easily inform patients of service improvements and developments, and have this communicated via relevant channels.
Insight and Involve (consult and engage):
Understand issues and ask for people’s opinions on ideas for change.
Goals:
- Develop a system of collating and analysing patient feedback from multiple sources (FFT, surveys, complaints, suggestion boxes, community forums, inpatient digital survey) as ongoing feedback to help inform service changes.
- Create an information pack for teams to have a standard approach for involving PPPLE.
- Develop a central register of already established community groups and people that could contribute in providing insight into our services.
Improve (co-design and co-produce):
Design and work together with people incorporating their ideas into the final approach.
Goals:
- By providing services that are accessible and inclusive for all through collaboration with key stakeholders.
- Develop a working with people policy (including assurance mechanisms).
- Develop a training programme so our staff understand how/when to work with people to get the best from the interactions.
- Collate evidence of improvement work that has been co-designed/co-produced
The introduction of a Co-production and Lived Experience Lead in 2023 will ensure the delivery of the above objectives.
National work
Parliamentary Health Service Ombudsman (PHSO) Complaint Standards Framework
The Trust commenced a review of the complaint process in line with recommendations from the PSHO, towards the end of 2022. The Stage 3 revised process went live in January 2023 and a work plan was developed to ensure other stages and associated processes are fully reviewed by the end of Quarter 2, 2023-2024.
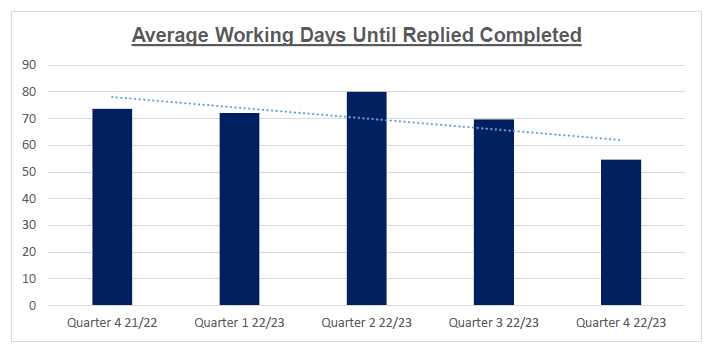
Initial results below are extremely positive, indicating a decrease in the number of working days from receipt to completion of a written response following a review of this process:
National Patient Safety and Incident Response Framework (PSIRF)
Work commenced on a framework to develop and maintain effective systems and processes for responding to patient safety incidents for the purpose of learning and improving patient safety, PSIRF replaces the Serious Incident Framework. There will be no distinction between patient safety incidents and ‘serious incidents’ (PSIRF covers ALL incidents). PSIRF promotes a proportionate approach to responding to patient safety incidents by ensuring resources allocated to learning are balanced with those needed to deliver improvement, it fundamentally shifts how the NHS responds to patient safety incidents for learning and improvement.
Moving forward into 2023-24 the principles of PSIRF will be used as a foundation in supporting complaint reviews within the Trusts patient experience teams, to ensure, we involve, engage and collaborate with patients, carers and the public in ensuring improvements are made where we have lessons to be learnt. We have recently adopted the swarm huddle process to ensure early engagement with all staff involved in patients care.
Local collaboration
We continue to enhance collaborative working with local organisations, which include:
Hartlepool Borough Council
Recently contributed to the development of a Joint Sensory Support Plan co-produced with local stakeholders following engagement with people who have a sensory loss or are Deaf and resident in Hartlepool.
South Tees Hospitals
Collaboration on the process to resolve early resolution complaints to align the processes where possible.
Accessibility partners
Involvement and collaborative working with our community partners which include Healthwatch Stockton, Healthwatch Hartlepool, North East Independent Complaints Advocacy Services, the Deaf Centre, Hi-Viz UK and the Trust’s interpreting and translation contracted supplier.
Regional complain managers forum
Led by North East Ambulance Service to share experience, discuss issues and work together to share good practice.
Integrated Commissioning Board (ICB)
During 2023-2024 the Trust will work collaboratively with the ICB to contribute to a Platform for Collaboration. This is a place for data capture across the learning journey creating a library of resources to share and develop. The programme will encourage thinking cleverly and building upon and sharing what organisations already have – for example a dignity framework, where older people observe the care of other older people. The key is to share good practice onto the Platform for the benefit of the Collaboration.
Training – Responding to complaints
We have reinforced the importance of fair and thorough complaint investigations with evidence of actions and learning with key personnel within the Trust by investing in externally delivered Responding to Complaints training. This has complimented the complaint process review.
Learning from the training includes:
- Triage with the complainant is key.
- We need to stop the internal ping pong between teams when attempting to finalise a complaint response.
- We need to avoid prolonging distress to complainants by continually attempting to resolve complaints, where this has been unsuccessful, and refer on to the PHSO, in line with the PHSO recommendations, for an independent complaint review.
Further external training sessions in Responding to Complaints will be undertaken during 2023-24 including a training session delivered to the Trust Board.
Online training opportunities for all staff involved in complaints management is available facilitated by the PHSO.
From Ward to Board
We are making it easier for patients and service users to contact us. There is a variety of ways they are able to provide feedback:
- Compliment
- Complaint
- Patient story
- Friends and family test return
- Local survey
- National survey
- Patient and carer experience council
- Healthcare user group
- Accessibility meeting
- Maternity and neonatal voices partnership
Patient Story
A patient story is presented during every Board meeting, this is usually a video recording, followed by the improvements made in light of the story – you said, we did. An example is Appendix A in this report.
Maternity Voice
North Tees and Hartlepool Maternity and Neonatal Voice Partnership (MNVP) is a growing team of service users, service user representatives, midwives, maternity staff, doctors and commissioners working to review and contribute to the development of local maternity and neonatal services. The current service user leads have been in place since September 2022 and so far we have been working to establish and build the team. This has been done via service user engagement sessions and working with local partner organisations, like Food and Baby Banks, and Parent and Toddler Groups.
We prioritise not just reaching out to the community but going out to them in the places they feel comfortable and safe to gather their feedback and amplify their voices. We collaborate with local charities to ensure we are hearing from those who would otherwise have to fight to be heard. Feedback is obtained in person at various groups in addition to via our social media pages, an online questionnaire, paper questionnaires at in-person events, and quarterly formal MNVP meetings.
Our current priorities for 2023/24 are to build the MNVP team with a hope of establishing focus groups to address infant feeding and bereavement care. Key to our work is truly listening to the person or people in front of us, empathising with them, empowering them and ensuring that their concerns are addressed. Our roles are underpinned by an awareness of trauma-informed care as evidenced by our Birth Trauma training, in addition to upholding human rights in maternity care as evidenced by our Birthrights training.
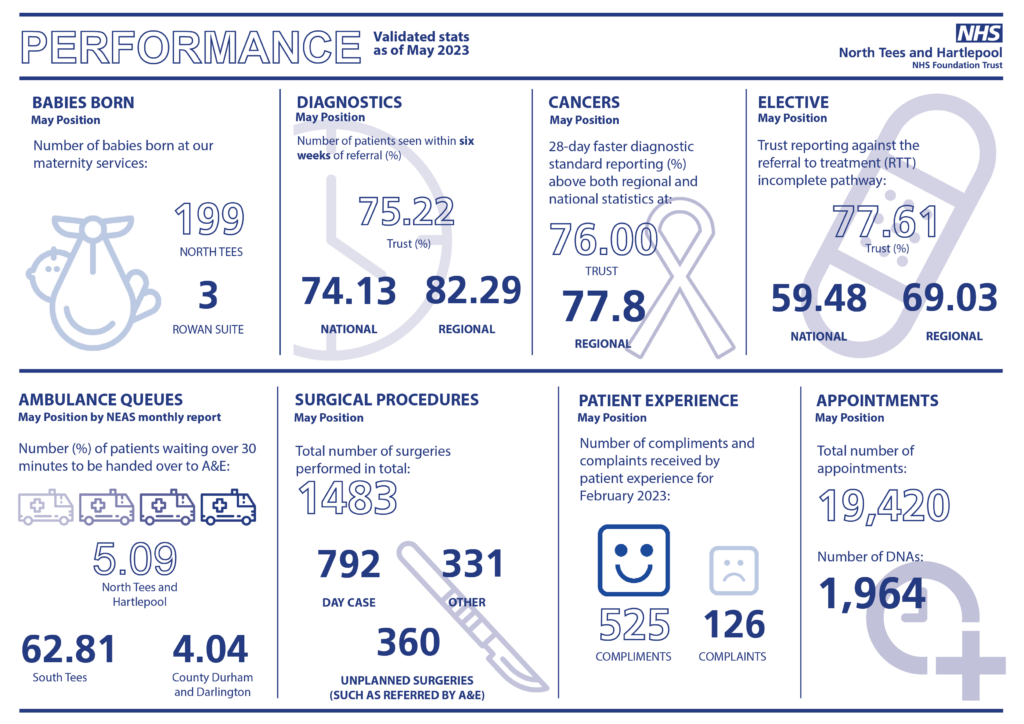
Performance reporting
The Trust Board receive a regular data including complaint and compliment numbers –
2. Complaint definitions
Stage 1
Local resolution, staff in the ward or department are requested to contact the complainant to resolve the complaint. The target is 7-working days, either face-to-face or via the telephone.
Stage 2
Following an investigation by the Care Group responsible to resolve the complaint, a meeting with senior staff is arranged. The meeting is arranged by the Care Group and can be face-to-face or virtual.
Stage 3
An investigation is undertaken and a written response is provided by the Care Group to be reviewed and approved by the Chief Executive or nominated deputy.
3. Complaints received by year by stage
| Stage | April 2020 to March 2021 | April 2021 to March 2022 | April 2022 to March 2023 |
|---|---|---|---|
| Stage 1 | 971 | 1208 | 1277 |
| Stage 2 | 46 | 98 | 114 |
| Stage 3 | 153 | 140 | 125 |
| Total | 1170 | 1446 | 1516 |
The advantage of resolution at Stage 1 means that concerns are addressed by the ward or department at the time the concern is raised or within a short period of time. The Trust resolved 83% of Stage 1 concerns in 2020-21, 84% in 2021-22 and 84% in 2022-23.
4. Top four themes by stage (all sub subjects)
Stage 1
2022 to 2023
- Communication
- Attitude of staff
- Length of Time to be Given an Appointment
- Treatment and Procedure Delays
2021 to 2022
- Communication
- Attitude of Staff
- Care and Compassion
- Treatment and Procedure Delays
2020 to 2021
- Communication
- Attitude of Staff
- Treatment and procedure Delays
- Care and Compassion
Stage 2
2022 to 2023
- Communication
- Care and Compassion
- Failure to Monitor
- Treatment and Procedure Delays
2021 to 2022
- Communication
- Attitude of Staff
- Care and Compassion
- Treatment and Procedure Delays
2020 to 2021
- Communication
- Care and Compassion
- Treatment and Procedure Delay
- Delay to Diagnose
Stage 3
2022 to 2023
- Communication
- Competence of Staff Member
- Timeliness of Discharge
- Treatment and Procedure Delay
2021 to 2022
- Communication
- Attitude of staff member
- Treatment and Procedure Delay
- Care and compassion
2020 to 2021
- Communication
- Treatment and Procedure Delays
- Delay to Diagnose
- Competence of staff member
Complaint themes are closely monitored and discussed during weekly Safety Panel Meetings and Senior Clinical Professionals Huddles. Where a trend is identified, actions are agreed and support is offered.
5. Response to the complainant provided within agreed timeframes
| Timeframe | Response rate (%) |
|---|---|
| April 2021 to March 2022 | 98 |
| April 2022 to March 2023 | 88 |
The data highlights that the percentage of complaints responded to within agreed timeframes is lower than the previous year.
To ensure this rate increases, improvements have been made throughout the complaint process review, this includes written confirmation of issues to be addressed with each complainant, the introduction of swarm huddles to agree terms of reference and ensure timescales for response are appropriate, early senior quality lead input to improve the quality of written response at a much early stage in the process. Additionally, improved communication between the Trust and the complainant, particularly a mid-point update of progress of the investigation, and contact from the Care Group where a response timescale will not be met to discuss the reasons for the delay and, if appropriate, a revised deadline may be agreed.
6. Outcome classification of Stage 3 complaints
All stage 3 complaints are reviewed following investigation to identify if the concerns were upheld, partially upheld or not upheld. Of the complaints closed at the time of reporting (June 2023):
| April 2022 to March 2023 outcome | Rates (%) |
|---|---|
| Not Upheld | 27 |
| All or some concerns were upheld | 73 |
There has been a slight increase in complaints partially or fully upheld when compared with the previous financial year (2021-22, 63%).
7. Actions and improvements undertaken 2022 – 23
Trust wide – Patient Experience Team led initiatives
Review of the Trust complaint process:
A review of the Trust’s complaint process in line with the PHSO Complaint Standards Framework commenced. The PSHO aims to ensure there are one set of Standards and one procedure for NHS organisations to follow, with a focus on working together to support colleagues to resolve complaints and identify learning and improve services for everyone.
Working relationships between all staff directly involved in complaint management has continues to be strengthened, particularly through the Complaint Process Review meetings and Complaint Panel meetings implemented with key stakeholders as part of the review process. The meetings provide an opportunity to discuss complex complaints, discuss process and gives an opportunity for clinical supervision.
Patient stories:
Patient feedback includes capturing patient stories. This includes the introduction of video recorded patient stories which captures learning and actions taken by the Trust to improve our services. The digital stories are presented at various forums including the Trust Board.
CQC National Survey Action Plans:
The process to ensure the development of adequate action plans following CQC National Surveys has been improved, with Surveys presented at the Patient & Carer Experience Council and a timescale agreed for Care Groups to present actions plans. This provide assurance of learning and improvement.
People, Patient and Public with Lived Experience Group (PPPLE):
The working Group was set up during 2022-23 to improve engagement and patient feedback. Work commenced on a plan to improve working in partnership with people and communities to inform, consult (insight and engage), improve (co-design and co-produce our services). A central stakeholder register has been devised and work is continuing to develop this. The stakeholders will input into service improvements within the Trust. The role of the PPPLE Lead commencing in Quarter 2 2003-24 for a fixed term period, will support in embedding this work.
Friends and Family Test:
The Trust’s Friends and Family feedback continues to utilise a text based methodology to allow for truly anonymous feedback. Patients receive a text message the day following discharge from the organisation. Responses are available via Yellowfin Dashboard. The Trust also provide paper based forms and this data is fed into Yellowfin. This improves accessibility in relation to options for patients in providing feedback. A pilot was carried out in the Accident and Emergency Department with the Trust volunteers who were present in the department to encourage and support completion of feedback forms with patients. This was successful as indicated in the table below which shows a significant increase in returns. Work is ongoing to recruit additional volunteers to assist in other wards and departments.
| Accident and emergency FFT returns | April 2022 to March 2023 | April 2023 to August 2023 |
|---|---|---|
| Total | 848 | 1269 |
Accessibility of our services:
Our Accessibility journey continues to ensure our patients receive equal access to and equal experience of our services. Patients and carers who use our services may require reasonable adjustments because of hearing impairment, visual impairment, learning disabilities, autism, Mental Health issues, sensory impairment, physical impairment, progressive condition or because their first language is not English. An Accessibility Meeting is in place and receives feedback in relation to good practice around accessibility. We introduced Accessibility Champions to work within our services to promote awareness of accessibility and provide guidance to staff. Discussions commenced around an Accessibility Lead to support his work on a fixed term basis.
A Disability Discrimination Act audit was commissioned and undertaken in 2022-23. Areas identified for improvement have been risk assessed and categorised. Initial funding was secured to commence the work and a work plan is under development for 2023-24.
The Trust’s external website has been developed to ensure compliance with the Accessible Information Standard regulations.
Live Digital Survey:
Work commenced to develop a live digital survey for inpatients to complete whilst on site just prior to their discharge. This will give a wealth of information by asking if the communication during a patient’s experience was sufficient, were staff friendly and understanding, was the patient involved in decisions around their discharge and how they rate their stay overall. A platform to collate and report this data has now been identified and the Information Technology and Digital Team are in the final stages of developing this.
Family Liaison Officers (FLO):
FLO’s are in place to support patients, families and carers during serious incident investigations. The aim of the FLO is to be the main point of contact throughout the investigation process, ensuring that families are supported sensitively and compassionately, giving them a chance to ask any questions. FLOs will work closely with the investigating team to be able to share timely and accurate information with openness and transparency. Training is ongoing to increase the number of FLO’s.
Care Group 1 – Healthy Lives (Out of Hospital Services and Women and Children’s Services)
Out of Hospital Services:
- New referral route via ICE for consultants to refer to adult community Speech and Language therapy Team which has reduced the time to receipt of referral.
- Partial booking text in physiotherapy – text messages sent to patients on the waiting list to see if they still require their appointment, this has significantly reduced wait times.
- Reducing waiting times for initial contact of patients referred for gestational diabetes by providing faster access to nutritional information via video.
- New trapeziectomy clinic in plaster room – reduced overbooking of dressings clinics and improved patient journey (reduced waiting times in clinic).
- New telephone MRI review clinic for scaphoid fractures – reduced face to face contacts, has patient experience and environmental benefits.
- Text reminder service in Tees Community Dental service – this has reduced time and cost associated with calling patients, also allowing patients to respond in a timely way.
- Integrated Musculoskeletal (iMSK) – New Trigger finger one stop clinic. Led to improved patient pathway – patient receives the treatment they need in fewer appointments, reduced waiting times, improved capacity in MSK to see other patients.
- iMSK – New Knee one stop clinic in place.
- New pathway implemented for Asthma discharge bundles – improved rate of bundle completion prior to discharge.
- Patent initiated follow up iMSK – new PIFU pathway across iMSK services has been introduced.
Women and Children’s Services:
- Accurate measurement of blood loss to support early detection of the deteriorating women at delivery.
- A new Post-Partum Hemorrhage (PPH) risk assessment has been developed and piloted within maternity to help with treatment and reduce the number of major PPH.
- New 12 Quit Programme has been implemented in Hartlepool and Peterlee to align with the services offered in Stockton. This will offer continued support for women in to quit smoking in pregnancy and reduce risks associated.
- The implementation of uterine artery Doppler scan for high risk women as part of the 20 week anomaly scan to early identify those women at risk of Small for gestational age babies.
- Training of staff in fetal bedside scanning to help with reduction of undiagnosed breech the aim is to have 70% of staff trained by October we currently have 60%.
- New procedure has been developed for medical ward handovers on pediatrics.
- Sophie’s legacy – this has been implemented within pediatrics and the catering department following feedback from families.
- ‘We can talk’ training (using co-production to improve the experience of children and young people who attend hospital due to their mental health and the staff who support them) has been introduced for all pediatric staff.
- Implemented the pre-term optimisation toolkit to improve outcomes for pre-term babies.
Care Group 2 – Responsive Care
- Participated in the review of the Trust’s complaint process.
- Developed of our leaders for the future by empowering and engaging with the launch of the Matron’s Handbook.
- Improved the Friends & Family return rate by engaging with patients in relation to feedback once identified as ready for discharge.
- Supported staff in attending FLO training and updates.
- Reduced wait times for patients requiring initial consultations, therefore receiving treatment sooner, promoting a more efficient service and patient journey.
- Inpatients have access to patient community to establish a continuation of co-ordinated care.
- Developed a passport for patients with a Hickman line to ensure safe and effective care during this hospital stay.
- Successful pilot of an alternative workforce model with the Respiratory wards to include a physiotherapist as part of the multi-disciplinary team.
- Reduction in dexa scanning reporting delays following completion of the reporting training for a Trust radiographer.
- Implementation of the ICC (Integrated coordination centre) to co locate the Discharge team and Patient Flow team together to predict, plan and optimise patient flow with proactive decision making.
Care Group 3 – Collaborative Care
- Participating in the review of the Trust complaint process to ensure it is in line with the PHSO Complaint Standards Framework and is actively updating the Care Group throughout the process.
- The weekly Care Group Patient Safety & Quality meeting is now well embeded and has very good attendence. The meeting was set up in response to staff feedback, to improve the sharing of complaints and incidents and identify any themes.
- The development of the Matron Handbook is now complete and all band 7 have engaged with the process.
- The Midline service continues in collaboration across the trust, supporting training and development to improve inpatient and outpatient pathways.
- We continue to use National Audits to drive Quality improvements (e.g. National Emergency Laparotomy Audit data) and achieved Gold award for the 2nd year running for the National Joint registry.
- Friends and Family Test results are reviewed weekly during the weekly patient safety meeting, addressing feedback and sharing with teams along with compliments on Yellowfin.
- Operationally, the Care Group continue to work on the ‘recovery programme’ to reduce waiting times for outpatient appointments and elective surgery.
- The Collaborative Care Group Conference was very well attended in 2022. Discussions included:
- Midline Service
- Learning from Never Events
- Lumen eye
- Theatre Robotics
- ACCP 1st year in post
- Radiology Consultant Practitioner Development
- ANP Introduction to 24/7 Nurse led service in Elective Care
- Emergency Gall Bladder Surgery: The New Norm?
8. Proposals and continued improvement in 2023 – 24
Trust-wide
- Development of a Patient Experience Plan on a Page for 2023-25.
- To continue to promote Reasonable Adjustments and develop a Policy.
- Improve recording of actions and learning from complaints.
- To implement a digital platform to encourage increased patient feedback via short surveys and digital option to submit patient stories.
- To enhance governance around patient safety and experience with the introduction of a new assurance system which allows triagulation of data (Inphase).
- To review the remaining sections in the PHSO Complaint Standards Framework – Financial Remedy, Stage 1 complaint process, Vexatious complainants.
- To work in collaboartion with South Tees with regard to aligment of some complaints processes.
- To enhance co-production with the patient experience partner role to help support the shaping of services taking into account patient experience and learning from feedback.
- To continue to develop a central register of service users who are willing to engage with Care Groups in service improvements.
- To continue to work with the Trust Volunteer Co-ordinator to continue to identify opportunities for volunteers to support patient feedback.
Care Group 1 – Healthy Lives
Out of Hospital Services:
- Self-care resources website for Musculoskeletal conditions – to support patients on or pre referral/whilst awaiting their appointment.
- Piloting different working time patterns in west wing to improve ability to carry out washing and dressing assessments in the aim of reducing the support/care required on discharge.
- To establish a pathway for high risk foot patients to be referred for midline insertion and administration of antibiotics in the community hub reducing the number of admissions.
- Managing Heart failure at home – providing heart failure patients with a digital based solution to enable greater oversight and improved management of their condition.
- Tobacco dependency – Vape pilot – to increase the engagement with the service and also quit attempts.
- New Tees Valley combined paediatric spinal Multi-Disciplinary Team – improved management of patients requiring input from paediatric spinal orthopaedic consultant.
- New GCA pathway – reducing the number of patients requiring a biopsy to confirm diagnosis.
- Early mobilisation post hip fracture – work ongoing to improve the number of patients mobilised within 24 hours of hip fracture surgery.
- Review of Community Nursing insulin administration processes.
- Ongoing development of virtual ward pathway and North East Ambulance Service stack work.
Pharmacy:
- Project currently piloting the benefits of Pharmacist working in the stroke/TIA clinics.
- Development of a new role for a Frailty Pharmacist working with the frailty team and on the Virtual Frailty Ward. This is to reduce harm from medicines and improve patient outcomes in people living with frailty.
- Pharmacy waste management project is currently underway and being piloted on EAU with the aim of reducing medication waste. Working with patients to ensure they bring their own medications into hospital and that they are transferred with them on their patient journey. This will be transformational and if works well will be implemented trust wide.
Women and Children’s Services:
- Supporting women on admission to quit smoking in pregnancy.
- Implementing mechanical induction of labor to improve patient experience.
- Working collaboratively across the care groups to improve the Child not Brought to Appointment Policy.
- Support women who deliver pre-term to give expressed breast milk within 24 hours to improve outcomes.
- Review of Cancer of unknown primary elective surgery pathways.
Care Group 2 – Responsive Care
- Implementation of safety checklists within assessment areas to ensure quality and safety standards continue to be maintained.
- Introduction of Nutrition and Hydration rounds within the Emergency Department and Emergency Assessment Unit, supported by our volunteers and Team Support Workers.
- Leadership within the Emergency Assessment Unit has been increased with a pilot of an additional Matron to allow continued senior visibility and oversight of patient quality and safety.
- Implementation of a Matron for both Children and Young People Emergency Department and the Emergency Departments to enable 7-day cover across both departments.
- Care Group representation within the NHSE QSIR (Quality, Service Improvement and redesign) training.
- Implementation of the Cancer Care co-ordinator role in all tumour groups to support the specialist nursing teams with the personalised care agenda.
- Collaborative working with North East Ambulance Service to ensure our ambulance handovers area as seamless a possible to allow the patients to be transferred to our Emergency Department as safely and timely as possible.
Care Group 3 – Collaborative Care
- To continue to participate in the review of the Trust complaint process to ensure it is in line with the PHSO Complaint Standards Framework and is actively updating the Care Group throughout the process.
- The 3rd Collaborative Care Group Conference went ahead on 7 July 2023.
- Getting it Right First Time (GIRFT) visit at the University Hospital of Hartlepool Hub took place on 10 July 2023 and the Collaborative Care team are working towards accrediatation.
- The Care Group continue to reduce stage 3 written responses and encourage face to face or local resolution.
- The following education and training is being rolled out withing the Collaborative Care Group as part of the trust initiative:
- Family Liaison Officer (FLO) training
- Bond solon complaint training
- Patient Safety Incident Response Framework (PSIRF)
- The on-going Patient Safety training and education will enable the Care Group to:
- Give patients and families the oportunity to be involved in investigations and encourage them to share their stories.
- Following the outstanding quality initiative and appreciative support visits feedback provides the ward/department with any learning, themes and good practice. This is shared across the Care Group.
- Improve the recording of actions and learning from complaints.
- Support patients, families and staff through the investigation process.
9. Further contacts received following a stage 2 or 3 complaint response
| Timeframe | Complaints received |
|---|---|
| April 2021 to March 2022 | 35 (Number of complaints received – 1446) |
| April 2022 to March 2023 | 32 (Number of complaints received – 1516) |
The percentage of further contacts decreased from 2.40% during 2021-22 to 2.11% in 2022-23.
10. The parliamentary and health service ombudsman (PHSO)
As an early adopter by the PHSO for the implementation of the Standards, this allowed early access to the Standards and to a support platform.
A Trust Complaint Improvement Project team have redesigning the complaint process. The stage 3 complaint process was implemented from 3 January 2023. Initial evaluation has shown positive results. The stage 2 process has been reviewed and work is well underway to finalise the stage 1 process.
The PHSO welcomes early signposting to them where a complainant remains dissatisfied following attempted resolution through the Trust’s complaints process. The complainant may choose to request an independent investigation/review of the complaint from the PHSO, the PHSO use their Standards when undertaking the investigation.
Cases reviewed by the PHSO
For reporting purposes once the Trust has received the scope of investigation provided by the PHSO, this is classified as a complaint that is under investigation by the PHSO.
There were 6 scopes of investigation received during 2023-23 and 3 cases closed by the PHSO. There were no cases upheld or partially upheld.
It is noted that the PHSO paused their investigation of complaints during the Covid 19 pandemic, this resulted in very low reporting figures in 2021-22 as indicated below when no Scopes of investigation were received and only 1 case closed. It is therefore difficult to compare data for both financial years.
| Timeframe | Scope of investigation received | Cases closed by PHSO | Cases upheld or partially upheld by PHSO |
|---|---|---|---|
| 2022 – 2023 | 6 | 3 | 0 |
| 2021 – 2022 | 0 | 1 | 0 |
11. Patient satisfaction surveys
Local Surveys 2022-23
We regularly carry out local patient surveys where patients, relatives, and carers are asked about the quality of the healthcare we have provided.
A selection of local surveys carried out 2022/23 include:
Endoscopy Patient Survey 2022
Annual survey that contributes to the unit’s annual Joint Advisory Group accreditation. Key results:
- 87% of patients were felt that this waiting time was about right.
- 95% were given a date and time for their endoscopy that was convenient for them.
- 98% were dealt with promptly and efficiently upon arrival to the unit.
- 93% stated that they had enough privacy during their endoscopy procedure.
- 89% received explanations about the procedure in a way they could understand.
- 84% received an understandable explanation of their results.
- 91% felt they were treated with respect and dignity by unit staff.
- 96% of patients would be extremely likely or likely to recommend the unit to friends and family.
Improvement plan:
To ensure patients know how long they are likely to wait for their procedure once they arrive on the unit, and to keep them updated if there are any delays.
A selection of comments:
“Very relaxed and all the staff were lovely. They were very understanding about me feeling anxious and nervous too, totally put me to ease.”
“I was very impressed with this unit, team work was of the highest standard along with high standards by any individual member of staff. I felt comfortable, relaxed and cared for.”
Women’s Health Counselling Service 2022
Continuous survey to ask women about the support and help they have received from this service. Key results:
- 70% of women felt they were referred to the service at the right time. 100% of women felt they felt listened to and 98% could explore other issues within the counselling appointment.
- 96% received privacy during their appointments. 100% felt that their sessions were very helpful.
A selection of comments:
“She taught me life skills I will never forget. It has transformed my life.”
“Right from the start I felt at ease with Julie, she was so warm and caring and actually listened to me.”
“I cannot put into words how grateful I am.”
“I would not have made it through without her.”
“She helped me to organise how I felt and things I could do to help myself feel differently, also to acknowledge I needed to allow time for this grief. I am very grateful for the time and care I received.”
Rapid Diagnostic Service Survey 2022
Survey to understand the impact this new service has had on patients. This service is a made up of a specialist team of health professionals who make sure the right diagnostics are rapidly performed for patients presenting with non-specific symptoms.
- 87% received an initial call from the RDS to explain how they would be involved and what would happen next in their care.
- 90% of patients who were given enough time to discuss their symptoms with the team.
- 93% of patients were given their results in a way they could understand.
- 90% were told what would happen to their care after they received their results.
- 97% were always treated with respect and dignity by the RDS team.
- 93% rated the care they received from the RDS as excellent, very good or good.
A selection of comments received:
“Felt good to have someone listen to his symptoms and felt he was being looked after.”
“I knew I was in safe hands and if my results were different I was confident I would be looked after.”
“Fast tracked and everything was really quick and straight forward.”
“The nurses were amazing as well as the consultants, they took their time and I felt like they really listened to me and what I was going through. They were very helpful and reassuring through the whole journey.”
Alcohol Care Team Survey 2023
Survey to gain understand experience of in patients who were seen and supported by this new service.
- 100% felt comfortable talking to the team.
100% were able to talk about their worries and concerns with the team. - 100% were given practical advice and support about how to reduce or give up alcohol.
97% were provided information about how to access other advice and support when they left hospital.
100% rated the care and support they received from the team as very good or good.
A selection of comments received:
“The lady was very professional, very helpful and spoke very clearly which is important as I am hard of hearing. She explained everything about the help I could get thank you.”
“The overall service from the alcoholic service was good. They know what they are talking about and genuinely care about the individual going through their journey from start to finish. I’d recommend anyone a chance at being happy.”
“Team referred me to the alcohol service and I am currently working with them with a view for a detox bed. Staff who have supported me were knowledgeable, compassionate and non-judgemental. Thank you.”
National Surveys 2022-23
The Trust take part in the mandatory National Patient Survey Programme which provides a way of measuring patient experience within our organisation, comparing our results over time, as well as assessing our performance with other Trusts. The coloured bars below show how the trust scored.
National Inpatient Survey 2021 (published October 2022) Key results
The Trust randomly selected adult inpatients discharged during November 2021. We had a 36% response rate with a total of 425 patients responding.
| Ares of good practice | Score |
|---|---|
| If you brought medication with you to hospital, were you able to take it when you needed to? | 8.7/10 |
| Thinking about your care and treatment, were you told something by a member of staff that was different to what you had been told by another member of staff? | 8.3/10 |
| Beforehand, how well did hospital staff answer your questions about the operations or procedures? | 9.3/10 |
| Did hospital staff discuss with you whether you may need any further health or social care services after leaving hospital? | 8.9/10 |
| After leaving hospital, did you get enough support from health or social care Services to help you recover or manage your condition? | 7.2/10 |
| Were you ever prevented from sleeping at night by noise from staff? (this question formed part of the Care Groups’ 2020 Action Plans) | 8.5/10 |
| Before you left hospital, were you given any information about what you should or should not do after leaving hospital? | 8.0/10 |
| Where we could do better | Score |
|---|---|
| How did you feel about the length of time you were on the waiting list before your admission to hospital? | 7.8/10 |
| To what extent did staff involve you in decisions about you leaving hospital? | 7.1/10 |
| Were you given enough notice about when you were going to leave hospital? | 7.2/10 |
| Thinking about any medicine you were to take at home, were you given any of the following? (Explanations about purpose, side effects, how to take, written info about medicines) | 4.1/10 |
A selection of comments:
“The staff were all brilliant & worked really hard even though COVID caused problems for the whole hospital.”
“The Doctors / nurses and staff were excellent and always there on call to help. Cannot fault any one of them BRILLIANT.”
“I was very impressed with the care I received whilst in hospital, I was especially impressed with the lengths taken by staff to respect my privacy and dignity in a difficult hospital situation. All the staff were very knowledgeable and professional.”
“Discharge arrangements weren’t great. I was left for most of the day being unsure what time I could leave or when. I got a sense of the nursing team being very busy and stretched as they coordinated a lot of patients individual discharge arrangement which took time.”
“I’m fully disabled and I have a big problem, I can’t sit down on the furniture that’s supplied in the shower, very inadequate.”
Action areas include
Admission to hospital – significant impact from pandemic on elective waiting lists. Extensive recovery programme with seven day operating in line with waiting list initiatives.
Explanation about how procedure/operation had gone – Pre Covid-19, patients were collected from day case/ward areas and relatives were involved in handover of information etc. This was restricted heavily during pandemic, particularly in the elective pathway areas to maintain the integrity of the areas. We have now reverted to pre Covid-19 business as usual. We have also developed our patient information leaflet offer, which was produced during Covid due to workforce and operation pressures.
Leaving hospital – Patients and family are now routinely involved in discharge discussions – this was challenging during Covid as lack of visitors etc.
National Maternity Survey 2022 (published in February 2023) Key results
Women aged 16 or over and who had a live birth in February 2022 were invited to take part in this survey. Our response rate was 39%.
| Areas of good practice | Score |
|---|---|
| Given support for mental health during pregnancy | 9.6 |
| Receiving appropriate advice & support when first contacted a midwife or the hospital at start of labour | 7.9 |
| Midwife or midwifery team were aware of their or their baby’s medical history (during care at home after the birth) | 8.7 |
| Being asked about mental health (during care at home after the birth) | 9.9 |
| Receiving support or advice about feeding baby, during evening/night/weekends (during care at home after the birth) | 7.4 |
| Midwives/doctors aware of medical history during antenatal check-ups | 7.6 |
| Midwives asking about mental health during antenatal check-ups | 9.2 |
| Midwives providing relevant information about feeding baby during pregnancy | 7.9 |
| Midwives/doctors aware of medical history during labour and birth | 8.0 |
| Where we could improve | Score |
|---|---|
| Being spoken to in a way they could understand during antenatal care. | 9.2 |
| Partners able to stay in hospital as much as they wanted | 2.8 |
| Attentiveness of staff during stay in hospital. | 7.8 |
| Being given information/explanations whilst in hospital. | 7.5 |
| Midwives/other health professionals providing active support and encouragement about feeding baby. | 7.8 |
A selection of comments:
“I can’t thank them enough for helping and supporting me and my partner during giving birth and my after care.”
“That I would like to thank everyone that helped me during my pregnancy and labour it was amazing experience.”
“I cannot fault the care I received from start to finish. Everyone I came in contact with was polite, understanding and happy to help. My whole pregnancy was a good pregnancy and knowing if something wasn’t right I had a lot of different services I could turn to for advice was reassuring.”
“I did not see the same midwife from 20 weeks of being pregnant. This was very upsetting as each time I had to explain my situation and each one had their own opinion. That was not helpful.”
“More information surrounding breastfeeding support & what to expect, how to know if breast feeding is successful would’ve been really useful and could have helped me avoid a hospital stay for failure to thrive. The midwife team who assessed growth scans were extremely understaffed and wait times were in excess of 3 hours at times.”
NB – An action plan from the Care Group to address areas we can improve will be developed.
National Cancer Patient Experience Survey 2021 (published July 2022)
All adult patients with a confirmed diagnosis of cancer discharged after an inpatient or day case patient attendance for cancer related treatment in the months of April, May and June 2021.
| Areas of good practice (where scores were higher than expected) | Score |
|---|---|
| Patient was told they could have a family member, carer or friend with them when told diagnosis. | 80% |
| Areas for improvement (where scores were lower than expected) | Score |
|---|---|
| Patient received all the information needed about the diagnostic test in advance. | 87% |
| Cancer diagnosis explained in a way the patient could completely understand. | 72% |
| Patient was definitely able to have a discussion about their needs or concerns prior to treatment | 67% |
| Staff provided the patient with relevant information on available support. | 82% |
| Patient was always able to discuss worries and fears with hospital staff. | 57% |
| The right amount of information and support was offered to the patient between final treatment and the follow up appointment. | 69% |
A selection of comments:
“Excellent, quick and I feel very lucky to live in an area where this level of treatment is possible despite ongoing NHS problems due to the pandemic.”
“I am very grateful that the care and treatment was administered as quickly as possible after diagnosis – no delays. The staff were all professional, caring and efficient.”
“Excellent. The staff at all levels were fantastic. Caring, cheerful, skill full and confident. Having bowel cancer, possible thyroid and lung cancer (still to be determined) is a horrible experience made better. By the doctors and nurses professional attitude. I don’t believe that they could have tried harder.”
“I feel so lucky and grateful to all of the staff that I have come into contact with during my treatment. Every person I was involved with, showed empathy and compassion throughout. Every single member of staff was kind, friendly and approachable as well as remaining professional. I can’t thank the teams enough. I felt listened to and they made a horrible situation, bearable.”
“Doctors’ practice – I am in this position because of the doctor & not being able to attend the practice during Covid. – I only had telephone appointments.”
“Test results haven’t always been on time, and sometimes communication, via the telephone, has led to delays. (Messages left, but not responded to, for example).”
“A little more information in regard to what to expect in terms of side effects and emotional feelings once chemo finishes.”
“Effects of hormone therapy could have been explained better (absolutely debilitating). After effects of operation could have been explained better. Still got pain and mobility problems and GP was absolutely no help at all.”
Action areas include
Patients not receiving enough information regarding diagnostic tests in advance – Ensure all relevant information leaflets are offered/given to the patient prior to test. We will do this by Working closely with Diagnostic centres to ensure this happens e.g. endoscopy and radiology. Cancer care coordinators with in the Rapid Diagnostic Service will speak with patients to ensure they fully understand when they need to attend appointments and to go through any questions they may have.
Cancer diagnosis not been explained in a way the patient could completely understand – Ensure there is a CNS present at diagnosis whenever possible. Ensure patients are given the cancer care coordinator contact details and are made aware of their role. The CNS will check that the patient has understood all information given at the end of the consultation.
Patients were not able to have a discussion regarding their needs or concerns prior to treatment. Improve shared decision making at the point of discussion regarding treatment – Ensure a CNS is present at the discussion where possible. The patient will be given the contact details of their cancer care coordinator and their role will be explained. A HNA will be completed along with a care plan tailored to each patient’s needs.
Staff did not provide patients with relevant information on available support – Cancer care coordinators are now in place to offer every patient support and guidance throughout their cancer journey. Every patient is now offered a HNA which is completed by the coordinators, any relevant referrals or signposted is done at this point and the patient knows the coordinator is their first point of contact throughout their whole cancer journey. Patients will be informed of any available support groups. Workshops are up and running for prostate patients who are appropriate for stratified follow up.
Patients weren’t always able to discuss worries and fears with hospital staff – Qualified staff oncology/palliative care training day to take place in September 2022 and March 2023. Visiting has reopened post pandemic to allow patients to have discussions with family members present. CNS teams have resumed their pre Covid duties including visiting the wards supporting patients and staff. Improve information available in ward areas for patients and relatives. Update notice boards in ward areas. Make ward areas aware of the role of cancer care coordinators so they know how to contact them if needed.
Survey feedback, action planning and review
A robust feedback strategy has been established where survey results are shared with key stakeholders in order to develop meaningful and achievable action plans. National survey results will be formally presented at the Patient and Carer Experience Council by the PET Survey Lead. The Care Groups will then be invited to present their action plans in 3 months for approval and sign off by the Committee. If there are any outstanding actions, the Care Groups will be invited to attend 6 months later to provide updates on the actions and service improvements.
The Patient Experience Team are working with the digital team to develop a patient satisfaction survey for patients to download via a QR code whilst they are onsite following an attendance or in patient stay. This is now in the final stages of the design phase with ongoing discussion about functionality and where and how the data will be stored, how data will be collated and displayed.
12. Overall compliment status
Since the introduction of Greatix within Datix in April 2020 staff have recorded higher compliment figures year on year.
This allows the Care Groups to review and share all compliment information received. All staff members are encouraged to record compliments. Compliment data now forms part of patient feedback thematic analysis.
Total number of compliments received
There were 4,612 compliments recorded during 2022-23 which is an increase of 547 on the previous year.
| Timescale | Compliments received |
|---|---|
| 2022 – 2023 | 4625 |
| 2021 – 2022 | 4065 |
| 2020 – 2021 | 2098 |
Total number of compliments by Care Group
Care Group for Healthy Lives
| Timescale | Compliments received |
|---|---|
| 2022 – 2023 | 1593 |
| 2021 – 2022 | 1167 |
Care Group for Responsive Care
| Timescale | Compliments received |
|---|---|
| 2022 – 2023 | 1211 |
| 2021 – 2022 | 1057 |
Care Group for Collaborative Care
| Timescale | Compliments received |
|---|---|
| 2022 – 2023 | 1754 |
| 2021 – 2022 | 1797 |
The Care Group for Collaborative Care has recorded the highest number of compliments with 1754 recorded during the last financial year, followed by Care Group for Healthy Lives and then Responsive Care.
Compliment themes:
2022 to 2023:
- Care Provided
- Compassion
- Staff to Staff
- Attitude
- Communication
2021 – 2022:
- Care Provided
- Compassion
- Attitude
- Staff to Staff
- Communication
Care provided continues to be the main theme in compliments followed by Compassion.
13. Overall friends and family test return rate
The NHS Friends and Family Test (FFT) is a valuable opportunity for patients to provide invited feedback on the care and treatment they receive in order to improve services. FFT asks patients whether they would recommend hospital services to their friends and family, if they required similar care or treatment. This means every patient in these wards and departments is able to give timely feedback on the quality of the care they receive.
The Trust offer paper based forms as well as a text based service to gather FFT feedback.
Friends and Family return rates (text based and paper based returns) 2022-23:
| FFT Response | Very Good | Good | Neither good nor poor | Poor | Very Poor | Don’t know | Total |
|---|---|---|---|---|---|---|---|
| Apr 22 | 1,138 | 183 | 30 | 24 | 23 | 3 | 1,401 |
| May 22 | 1,265 | 259 | 51 | 38 | 36 | 3 | 1,652 |
| Jun 22 | 1,281 | 229 | 51 | 37 | 37 | 5 | 1,640 |
| Jul 22 | 1,284 | 218 | 43 | 31 | 51 | 5 | 1,632 |
| Aug 22 | 1,410 | 231 | 58 | 31 | 35 | 2 | 1,767 |
| Sep 22 | 1,200 | 178 | 45 | 31 | 34 | 4 | 1,492 |
| Oct 22 | 1,479 | 236 | 53 | 24 | 53 | 3 | 1,848 |
| Nov 22 | 1,263 | 202 | 47 | 31 | 36 | 7 | 1,586 |
| Dec 22 | 1,170 | 205 | 32 | 31 | 53 | 7 | 1,498 |
| Jan 23 | 1,594 | 222 | 51 | 26 | 34 | 5 | 1,932 |
| Feb 23 | 1,640 | 242 | 53 | 31 | 31 | 4 | 2,001 |
| Mar 23 | 1,637 | 271 | 48 | 21 | 30 | 9 | 2,016 |
| Total | 16,361 | 2,676 | 562 | 356 | 453 | 57 | 20,465 |
The table above demonstrates that returns indicating Very Good and Good account for over 93% of the FFT response forms returned during the financial year 2022-23, this is an improvement of 1% on the previous financial year.
There has been an increase of 2,356 returns in 2022-23 compared with 2021-22:
| Response returns | 2021 – 2022 | 2022 – 2023 |
|---|---|---|
| Total returns | 18,109 | 20,465 |
| Percentage rating very good/good | 92% | 93% |
| Percentage rating very poor/poor | 4% | 4% |
Work continues to improve the return rate of FFT responses.
Appendix A.
A Family Story – Mr A regarding the care of his late mother, Mrs B.
Mr A wrote to the Patient Experience Team following the death of his mother Mrs B. Mrs B had end stage dementia. He and his family wanted to provide some feedback on the care his mother had received from the community district nursing (DN) team. Mr A articulated his concerns about the use of the Care of the Dying Patient (CDP) document and the Family Voice Diary. They felt that the document content was not explained or discussed with them or completed appropriately during the early stages to support Mrs B’s end of life care.
The family were only made aware of the Family Voice after Mrs B had passed away, and they felt that if they had an opportunity to complete this at the time it would have aided and supported communication with the district nurses. The family also felt that the CDP was not properly completed and updated, which led to inconsistent communications between the district nurses looking after Mrs B. This lead to the concerns regarding Mrs B’s pain management with perceived long periods of pain and agitation before district nurses would attend. The family felt that when the DN team attended Mrs B was often settled and so was difficult for the team to administer medication that the family felt was needed when they arrived.
The family cited specific DNs who they wanted to praise for the care and compassion, however, they wanted to ensure that the constructive feedback they provided about the use of the CPD and Family Voice Documentation would help other families in the future.
Following on from the concerns being raised the Nurse Consultant in Palliative and End Of Life (EOL) Care developed an eLearning package to support nurses to be empowered to share the family voice diary as soon as the care of the dying patient document was initiated.
To date across the DN teams 96% of band 6 DN sisters/ DN apprentices and DN students have completed the eLearning package. (Only one DN Sister and One DN student to complete). Wider teams also continue to access and complete the eLearning.
Mr A was so passionate around the importance of families being able to use the diary this year when he returned back to the UK for a holiday he met up with our communications team and the Associate Director of Nursing, Experience and Improvement to record his story. He was keen for the Trust Board to hear his story not just in relation to the concerns he raised but also to ensure that learning is shared across the trust at wider forums such as the EOL steering group too.
PDF Document download
Click the link below to view or download our Patient experience and involvement report 2022 – 2023:
Patient experience and involvement annual report 2022 – 2023 (1MB)
If you use assistive technology such as a screen reader and need a version of this document in a more accessible format, please email us at [email protected]