Information for patients
This leaflet can be made available in other formats including large print, CD and Braille and in languages other than English, upon request.
This leaflet tells you about nasogastric and nasojejunal tube feeding. Your doctor or nurse will discuss this with you and answer any questions you may have.
What is nasogastric feeding?
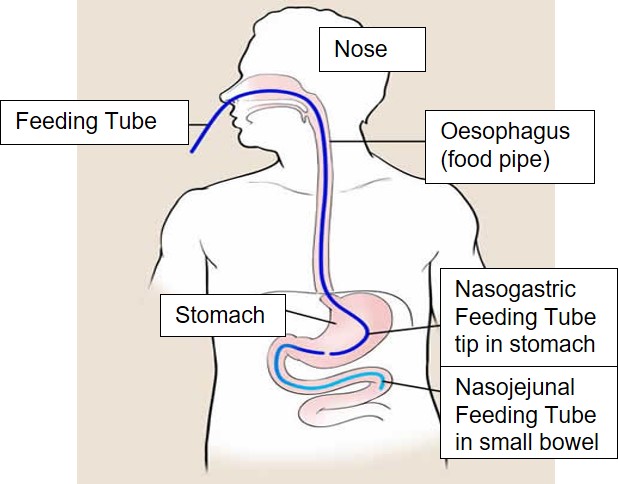
Nasogastric feeding is when a narrow plastic tube is placed through the nose, directly into your stomach (see diagram below). Once in place the tube can be used to give you liquid food directly into your stomach.
Why do I need a nasogastric tube?
There are several reasons why you may not be able to eat enough food normally at the moment. For example:
- You may have a problem swallowing, due to a stroke, Parkinson’s disease, motor neurone disease, cerebral palsy or other nerve conditions.
These conditions can make it unsafe for you to eat. This problem may mean a risk of food entering your windpipe and lungs causing pneumonia or a chest infection. - You may have a blockage at the back of your throat or in your oesophagus (gullet) which stops your food going down normally
- You may have lost your appetite due to another illness, which means you are not able to eat enough food.
How is the nasogastric tube inserted?
Although you may find this uncomfortable it should not hurt. The procedure is usually performed at your bedside or whilst you are in bed. You will need to sit up straight. A narrow plastic tube is lubricated with water and is passed into one of your nostrils. The tube passes to the throat and at that point you would be asked to put your head forward and the tube should pass into your food pipe (oesophagus). Sometimes we may get you to drink some water through a straw to help the tube to get into the food pipe. Once the tube is safely into your food pipe it will be gently inserted further into the stomach. The tube tip will sit 45-55cm (18-22in) from your nose.
Once the tube is inserted it will be held in place with a special plaster, surgical tape or occasionally a bridle device.
Are there any risks or possible complications of having a nasogastric tube inserted?
Nasogastric feeding is a safe procedure. There is a risk the tube may be inserted into the lung. If this happens you may cough and the tube would be removed. Sometimes a patient is unaware that the tube has passed into the lung so your doctor or nurse will always check the position of the tube before feeding. This position check is through obtaining an aspirate (sample) from the tube or doing a chest X-ray.
What is nasojejunal feeding?
Nasojejunal feeding is when a narrow plastic tube is passed up your nose, down your throat and into your jejunum (small bowel), (see Diagram 1 earlier in the leaflet). Once in place the tube can be used to give you liquid food directly into your bowel.
Why do I need a nasojejunal tube?
Sometimes food from the nasogastric tube stays in the stomach for longer than normal. This means:
- it can flow back up the oesophagus (gullet) and spill into your lungs. If this happens you will be at risk of pneumonia.
- the food will not reach the jejunum where your body absorbs food.
A nasojejunal tube places food directly into your small bowel so you will not have these problems.
How is the nasojejunal tube inserted?
It is more difficult to place a nasojejunal tube (than a nasogastric tube) as the tube tip has to pass through the stomach and into the small bowel. The tube can be placed using a gastroscope (a thin, flexible tube) which has a bright light and a camera at the end of it which passes back a picture on to a monitor or using X-ray.
Are there any risks or complications of having a nasojejunal tube inserted?
Nasojejunal feeding is a safe procedure. There are risks associated with an endoscopy, you will be given a leaflet ‘Upper gastro-intestinal (GI) endoscopy’ which explains this in more detail.
What happens after the tube is inserted?
When the tube is in the correct position it will be used to pass liquid food into your stomach or small bowel.
What will I be given?
You will be given liquid food which contains all you will need on a daily basis.
The food will be delivered either through a pump device that delivers food continuously over several hours or large volumes using a syringe 3 or 4 times per day.
The amount of food and delivery method will be decided by your doctor or nurse, depending on which is best for you.
You may also be able to eat some food normally.
You may be given liquid medication through the tube.
How will the feeding tube be cared for?
Sometimes the liquid food can harden and block the tube. To prevent this, the tube will be flushed with water before and after each of your feeds. The position of the tube will also be checked before each feed.
What happens if the tube becomes blocked?
If the tube becomes blocked attempts will be made to flush it with some water. If this does not work a new tube will need to be inserted.
How long will the tube need to stay in for?
This will depend on why the tube was inserted. Usually the tube will be used only for a short time (a few days to a couple of weeks) while you are in hospital.
Your doctor or nurse will be able to discuss this with you in more detail.
Further information is available from:
National Institute for Health and Care Excellence (NICE)
Further information at the NICE website.
PINNT (Patients on Intravenous and Nasogastric Nutritional Therapy)
PO Box 3126,
Christchurch,
Dorset,
BH23 2XS
Further information can be found on the PINNT homepage.
PINNT enteral nutrition information can also be found on the website: www.pinnt.com/Therapies/Enteral-Nutrition.aspx
Comments, concerns, compliments or complaints
Patient Experience Team (PET)
We are continually trying to improve the services we provide. We want to know what we’re doing well or if there’s anything which we can improve, that’s why the Patient Experience Team (PET) is here to help. Our Patient Experience Team is here to try to resolve your concerns as quickly as possible. The office is based on the ground floor at the University Hospital of North Tees if you wish to discuss concerns in person. If you would like to contact or request a copy of our PET leaflet, please contact:
Telephone: 01642 624719
Freephone: 0800 092 0084
Opening hours: Monday to Friday, 9:30am to 4:00pm
Email: [email protected]
Out of hours
Out of hours if you wish to speak to a senior member of Trust staff, please contact the hospital switchboard who will bleep the appropriate person.
Telephone: 01642 617617
Data protection and use of patient information
The Trust has developed Data Protection policies in accordance with Data Protection Legislation (UK General Data Protection Regulations and Data Protection Act 2018) and the Freedom of Information Act 2000. All of our staff respect these policies and confidentiality is adhered to at all times. If you require further information on how we process your information please see our Privacy Notices.
Telephone: 01642 383551
Email: [email protected]
Privacy NoticesLeaflet feedback
This leaflet has been produced in partnership with patients and carers. All patient leaflets are regularly reviewed, and any suggestions you have as to how it may be improved are extremely valuable. Please write to the Clinical Governance team, North Tees and Hartlepool NHS Foundation Trust, University Hospital of North Tees, TS19 8PE or:
Email: [email protected]
Leaflet reference: PIL
Date for Review: