Information for patients
This leaflet can be made available in other formats including large print, CD and Braille and in languages other than English, upon request.
Your doctor has advised you have a colonoscopy to:
- Help find the cause of your symptoms.
- As part of a routine surveillance programme to detect (find) disease or abnormalities (unusual areas) at an early stage in people with no symptoms.
- To follow up previous abnormalities.
This leaflet tells you about Colonoscopy and will help you to understand what will happen during and after your examination.
What is a colonoscopy?
A colonoscopy is an examination that allows an Endoscopist (a Doctor, Nurse or Physician Associate trained to do endoscopies) to see inside your large intestine (bowel or colon). This is the most accurate way of looking inside your bowel. The procedure includes a rectal examination, wherein the Endoscopist uses their finger to assess for any problems inside your back passage (rectum) prior to scope insertion. The rectal examination is usually very quick and should not cause you too much discomfort.
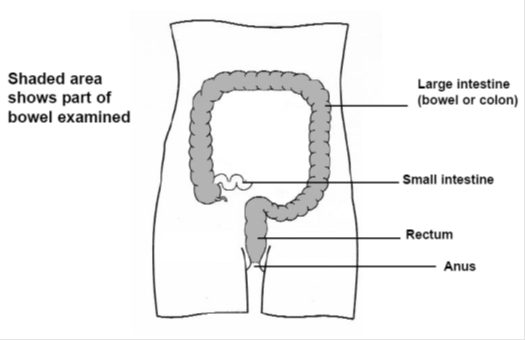
A colonoscope (a soft, flexible tube about the thickness of your finger) is passed into your rectum (back passage) and guided through your large intestine (see diagram). This tube has a bright light and camera at the end of it that passes back a picture of the inside of your bowel on to a monitor.
Your Endoscopist can then check if any disease or abnormalities are present. Biopsies (small pieces of tissue) can be taken and any polyps (small warty growths) can be removed for examination in a laboratory.
Polyps are not uncommon and are more frequent as we grow older. A quarter to a half of the population above the age of 50 will grow polyps7. Polyps up to 2 cm in size can be removed safely by all trained Endoscopists and are a routine part of the procedure. This can sometimes prevent bowel problems in the future.
What are the risks and possible complications?
Colonoscopy is generally a very safe procedure, but it does have some risks and possible complications. These will be discussed fully before you consent to the examination. They must be compared to the benefits of having the procedure carried out. The Doctor who advised you should have this procedure will have considered this.
The risks and possible complications include:
- Discomfort. You may feel some discomfort during the procedure; we try to keep this to a minimum. You can ask for the procedure to stop at any point if you wish
- Bloating. You may feel bloated for a few hours afterwards
- Bleeding. 1 patient in every 3861 can suffer rectal bleeding. This may need a blood transfusion, or rarely, an operation.
- The risk can increase if polyps are removed. If the bleeding happens during the test the Endoscopist will try to stop the bleeding with clips and injections. Sometimes bleeding can occur up to 2 weeks after the procedure.
- Perforation (hole). 1 patient in every 2,5111 can suffer a perforation in the wall of the bowel.1 The risk of perforation is higher with polyp removal. This can happen to 1 patient in every 1002 when large or complex polyps are removed. If a perforation happens, sometimes the hole can be closed with clips during the colonoscopy. If the hole cannot be closed an emergency operation is needed to repair it.
Sometimes, during the operation, a stoma (opening where the end of your bowel is brought out on to the skin of your abdomen (tummy) may be needed to allow your bowel to rest and heal. The stoma can usually be closed when your bowel has healed
- Adverse effects of conscious sedation (a drug which makes you feel comfortable and relaxed). Sedation can occasionally cause problems with your breathing, heart rate and blood pressure.
Careful monitoring (checking) by a fully trained Endoscopy Nurse will make sure any problems can be identified and treated quickly. If any side effects of the medication occur treatment can be given to reverse this in the department.
- Missed abnormalities. Colonoscopy is a very accurate examination but, as with any other test, occasionally a problem (including, rarely, a cancer) may be missed4,5,6.
- Incomplete test. There is also a possibility that the procedure will be incomplete and that the entire colon will not be examined as intended. In this case, your endoscopist or referring doctor will discuss alternative tests with you.
- Other treatments. Sometimes a person’s blood pressure can drop during the test and the team may need to give you a drip (into your vein) of fluid to treat this. Any unforeseen emergencies will be treated immediately.
Are there any other tests that can be done instead of a colonoscopy?
You do not have to have any examination or test you do not want, but the Doctor who has requested the examination has advised this is best for you.
If you do not want this examination, a CT Colonography (CTC) is an x-ray examination also known as a virtual colonoscopy which could help find the cause of your symptoms however, it provides slightly different information to a colonoscopy which may not be the best test for you.
If you decide not to have a colonoscopy you will need to let the Endoscopy Unit know before your appointment date.
If you decide you want a CTC scan you will need to go back to your GP surgery or your referring hospital Consultant and discuss the options available with them.
What will happen before my colonoscopy?
You will be admitted as a day case patient unless your appointment letter states otherwise. You will usually be able to go home 30 – 60 minutes after your examination. Very occasionally your doctor may advise you to stay in hospital overnight after your colonoscopy.
Before your examination you will be given sedation and a painkilling drug. This is called conscious sedation. You will still be awake but should feel more comfortable and relaxed.
This involves injecting medication (drugs), through a cannula (a fine tube) inserted into a vein in the back of your hand or arm using a small, fine needle.
What will I need to do to prepare for my colonoscopy?
It is very important your bowel is empty and clean otherwise it may affect what the doctor can see when your bowel is being examined and your colonoscopy may need to be rearranged. You mustfollow the instructions given in the leaflet provided.
You must also arrange for a responsible adult to take you home and stay with you for at least 12 hours after your examination, as the effects of the sedation will affect your judgement. If you have not made these arrangements and want to be sedated your colonoscopy will have to be postponed.
Please bring a dressing gown, slippers or flat shoes, a list of medications (drugs) you are currently taking, either prescribed by your Doctor or those you have bought yourself and your reading glasses with you on the day of your appointment. Please note you will need to bring in your own bag as the Unit do not provide these.
What will happen when I arrive for my appointment?
When you arrive at the Endoscopy Unit you will be told the approximate time you should be ready to go home. Anyone wishing to stay and wait for you will be shown where he or she can wait.
There is limited space in the unit, so only in special cases will anyone be able to stay with you, for example, adults with special needs.
A nurse will call you through to the unit, check your personal details, ask you questions about your health, check your blood pressure and pulse and explain the examination and risks to you. This is just to make sure you understand everything before you sign the consent form.
You should tell the nurse if you have had any allergies or reactions to drugs or other tests in the past and of any previous colonoscopies or flexible sigmoidoscopies you may have had.
We operate a list system. This means you will be seen when it is your turn and not the time given for you to arrive at the Unit.
Before your examination you will be taken to a private area and asked to remove some of your clothing. You will be given a gown and some modesty pants to put on, together with your dressing gown and slippers.
You may be taken to a waiting area with other patients or a private room to wait your turn. When it is time for your colonoscopy a nurse will take you into the examination room.
What will happen during my examination?
You will be taken into the examination room and made comfortable on the examination trolley/bed. The Endoscopy Team will confirm that everything is in order and give you a chance to ask any final questions before your test begins.
Before your examination begins, if you are going to have sedation, a cannula will be inserted into a vein in the back of your hand or arm using a small, fine needle. The sedative and painkillers will be given through the cannula just before your examination begins. This should help you to feel more comfortable and relaxed.
You will be asked to lie down on a trolley on your left side, with your knees slightly bent. A small plastic clip will be put on to one of your fingers to check your pulse and the oxygen levels in your blood, before and during your examination. You may be given extra oxygen to breathe through a soft plastic tube on your nose. Do not worry, this is all routine.
A nurse will stay with you during your examination and make sure you are comfortable.
Before the camera test begins, the Endoscopist will perform a digital rectal examination (examination of the back passage with gloved finger covered in lubricant jelly).
The colonoscope will then be gently inserted into your rectum and guided through your large bowel. Air and water will be passed through the tube to inflate your bowel so your Endoscopist can see all parts of your bowel wall. This can cause ‘windy’ discomfort. You may also feel you want to open your bowels but as they are already empty this will not happen.
The examination can take from 10 – 40 minutes to complete.
We routinely take photographs or videos of your insides during this procedure. These are used to help in your investigations and treatment. The pictures taken during your examination will be kept as part of your healthcare record.
The pictures may sometimes be used for training or research but would always be anonymised (they would have no details which could identify you). If hospital staff want to use any of your pictures for any other purpose, for example, in an article to be published (printed) in a professional magazine or book, they will ask your permission before this happens.
You will have been given a painkilling drug with your sedation before your examination begins, so usually this examination is not painful. However, you may feel some discomfort. If needed, you can also be given a special gas called Entonox to breathe. You can ask for the procedure to stop at any point if you wish.
What will happen after my examination?
You will be taken to the recovery area where you will be able to rest until the immediate effects of your sedation have worn off. After this you will be helped off the trolley and you can get dressed.
You will then be offered a hot drink and a snack. The person you have arranged to take you home will then be asked to come to the Unit to collect you. You will not be able to go home on your own. The effect of sedation will stay with you for at least 12 hours so it is important you follow this advice.
There must be a responsible adult to take you home and look after you for the first 24 hours after your examination, as the effects of the sedation will affect your judgement. Your nurse will tell you how long you need to follow this advice.
For the first 24 hours after sedation you:
- Must not go back to work.
- Must not drive a car, ride a bicycle or motorcycle. It is an offence to drive while unfit to do so because of the drugs used and it will probably invalidate your insurance policy.
- Must not supervise children.
- Must not make important decisions or sign any legal documents.
- Must not operate machinery or electrical appliances.
- Must not go near open flames or sources of high heat.
- Must not drink alcohol.
- Must not take sleeping tablets, tranquillisers or any drugs, other than those prescribed, for you by your GP.
- Must not lock the toilet or bathroom door in case you need any help.
- Should not smoke.
When will I be told the result of my examination?
Before you leave the unit your nurse or endoscopist will explain the results of your examination to you. If you have had sedation you may not remember everything you have been told so, with your permission, it may be helpful if a relative or friend could be with you when you are told your results.
You will also be given a discharge information leaflet. Your GP will be sent a copy of your results.
If you had any biopsies taken and sent to a laboratory for further examination you may have to wait for up to 6 weeks for the results.
You should contact your GP for these results.
If needed, you may be sent an outpatient appointment, through the post, to discuss the results of your colonoscopy in more detail. A copy of your results will also be sent to your GP.
How will I feel when I go home?
You may feel tired due to the effect of the sedation. Do not worry, relax quietly at home for the rest of the day.
You can eat and drink as normal after your examination. As your bowel has been emptied it often takes 2 – 3 days for your bowel movements to return to normal.
You can take your medications as normal. You may suffer from some abdominal discomfort due to the air put into your bowel during your examination. This may make you feel bloated and you may feel the need to pass wind. This usually settles within 24 hours.
If you had any biopsies or polyps removed, you may pass small traces of blood from your rectum for up to 48 hours after your colonoscopy.
You must contact the Endoscopy Unit (see contact numbers) where you had your endoscopy immediately if:
- You have severe pain in your abdomen.
- You develop a temperature higher than 38ºC (100.4ºF).
- You develop vomiting (being sick) or nausea (feeling sick).
- Any bleeding from your rectum increases or continues for longer than 48 hours.
If the department is closed and you have an urgent problem the night after your colonoscopy you should contact your local Emergency Department (see contact numbers)
Contact numbers
If you need further advice, or have any problems, please contact the appropriate number below:
University Hospital of North Tees
Endoscopy Unit
Telephone: 01642 624387
Monday to Friday 8am to 7pm
Emergency Department
Telephone: 01642 382899
24 hours a day, 7 days a week
University Hospital of Hartlepool
Rutherford Morrison Unit
Telephone: 01429 522356
Monday to Friday 8am to 6.30pm
If you have any worries or concerns, you should contact your GP during normal surgery hours.
Outside surgery hours you should contact your GP surgery for the Out of Hours Service number.
Further information is available from:
NHS Choices
Telephone: 111 (when it is less urgent than 999)
Calls to this number are free from landlines and mobile phones
or via the website at www.nhs.uk
References
- Gavin D, Valori R, Anderson JT, et al.
The National Colonoscopy Audit: a nationwide assessment of the quality and safety of colonoscopy in the UK. Gut 2013;62:242–9. - Panteris V, Haringsma J, Kuipers EJ.
Colonoscopy perforation rate, mechanism and outcome: from diagnostic to therapeutic colonoscopy. Endoscopy 2009;41:941-51. - Haycock, A., Cohen, J., Saunders, B., Cotton, P.B. and Williams, C.B. (2014). Cotton and Williams’ practical gastrointestinal endoscopy: the fundamentals. Chichester, West Sussex, Uk: John Wiley And Sons, Inc.
- Burr, N.E., Derbyshire, E., Taylor, J., Whalley, S., Subramanian, V., Finan, P.J., Rutter, M.D., Valori, R. and Morris, E.J.A. (2019). Variation in post-colonoscopy colorectal cancer across colonoscopy providers in English National Health Service: population based cohort study. BMJ, [online] p.l6090. doi:https://doi.org/10.1136/bmj.l6090.
- Rutter, M.D., Beintaris, I., Valori, R., Chiu, H.M., Corley, D.A., Cuatrecasas, M., Dekker, E., Forsberg, A., Gore-Booth, J., Haug, U., Kaminski, M.F., Matsuda, T., Meijer, G.A., Morris, E., Plumb, A.A., Rabeneck, L., Robertson, D.J., Schoen, R.E., Singh, H. and Tinmouth, J. (2018). World Endoscopy Organization Consensus Statements on Post-Colonoscopy and Post-Imaging Colorectal Cancer. Gastroenterology, 155:(3), pp.909-925.e3. doi:https://doi.org/10.1053/j.gastro.2018.05.038.
- Morris, E.J.A., Rutter, M.D., Finan, P.J., Thomas, J.D. and Valori, R. (2014). Post-colonoscopy colorectal cancer (PCCRC) rates vary considerably depending on the method used to calculate them: a retrospective observational population-based study of PCCRC in the English National Health Service. Gut, 64:(8), pp.1248–1256. doi:https://doi.org/10.1136/gutjnl-2014-308362.
- Rutter, M.D., East, J., Rees, C.J., Cripps, N., Docherty, J., Dolwani, S., Kaye, P.V., Monahan, K.J., Novelli, M.R., Plumb, A., Saunders, B.P., Thomas-Gibson, S., Tolan, D.J.M., Whyte, S., Bonnington, S., Scope, A., Wong, R., Hibbert, B., Marsh, J. and Moores, B. (2019). British Society of Gastroenterology/Association of Coloproctology of Great Britain and Ireland/Public Health England post-polypectomy and post-colorectal cancer resection surveillance guidelines. Gut, 69:(2), pp.201–223. doi:https://doi.org/10.1136/gutjnl-2019-319858.
Comments, concerns, compliments or complaints
Patient Experience Team (PET)
We are continually trying to improve the services we provide. We want to know what we’re doing well or if there’s anything which we can improve, that’s why the Patient Experience Team (PET) is here to help. Our Patient Experience Team is here to try to resolve your concerns as quickly as possible. The office is based on the ground floor at the University Hospital of North Tees if you wish to discuss concerns in person. If you would like to contact or request a copy of our PET leaflet, please contact:
Telephone: 01642 624719
Freephone: 0800 092 0084
Opening hours: Monday to Friday, 9:30am to 4:00pm
Email: [email protected]
Out of hours
Out of hours if you wish to speak to a senior member of Trust staff, please contact the hospital switchboard who will bleep the appropriate person.
Telephone: 01642 617617
Data protection and use of patient information
The Trust has developed Data Protection policies in accordance with Data Protection Legislation (UK General Data Protection Regulations and Data Protection Act 2018) and the Freedom of Information Act 2000. All of our staff respect these policies and confidentiality is adhered to at all times. If you require further information on how we process your information please see our Privacy Notices.
Telephone: 01642 383551
Email: [email protected]
Privacy NoticesLeaflet feedback
This leaflet has been produced in partnership with patients and carers. All patient leaflets are regularly reviewed, and any suggestions you have as to how it may be improved are extremely valuable. Please write to the Clinical Governance team, North Tees and Hartlepool NHS Foundation Trust, University Hospital of North Tees, TS19 8PE or:
Email: [email protected]
Leaflet reference: PIL1008
Date for Review: 12/07/2026