Information for patients
This leaflet can be made available in other formats including large print, CD and Braille and in languages other than English, upon request.
Your doctor has said you need to have a procedure called a coronary angiogram to find out more about your coronary arteries (blood vessels of the heart), heart valves and the pumping function of your heart.
This leaflet tells you about a coronary angiogram and will help you to understand what will happen during and after your procedure.
What is a coronary angiogram?
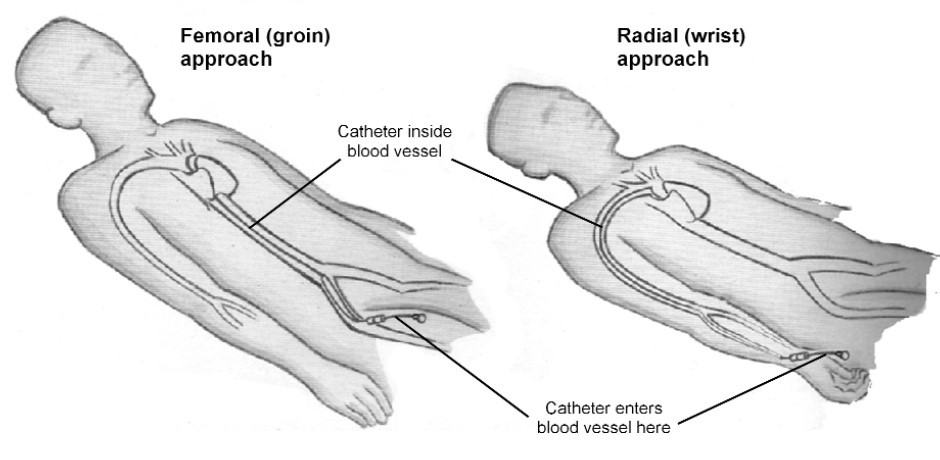
A coronary angiogram is a special X-ray of your coronary arteries. It can also be called cardiac catheterisation. The coronary arteries do not show up on ordinary X-rays. During an angiogram a very fine, long, special catheter (tube) is passed through an artery in either your wrist or groin until it reaches your coronary artery.
A special dye, called contrast medium, is injected through this catheter into your coronary arteries which then allows them to show up on an X-ray. See diagram 1.
The procedure will also give your doctor vital information about the blood pressure inside your heart, how well your heart is pumping and how the valves of your coronary arteries are working.
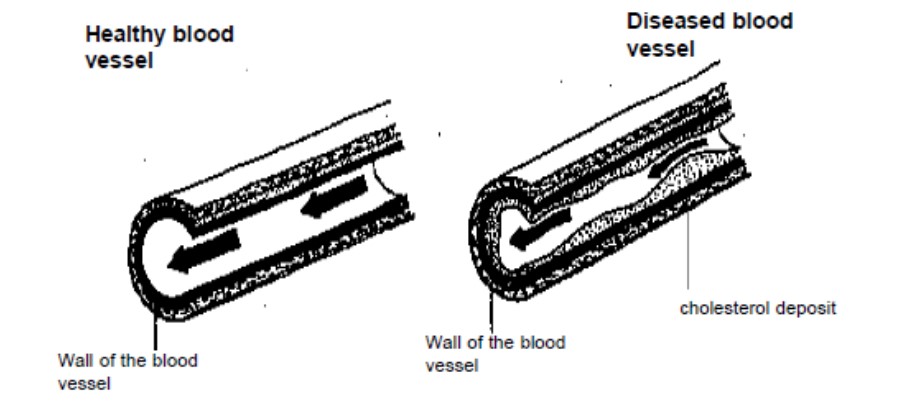
An angiogram can show if you have any narrowing of your coronary arteries and exactly where the narrowing is. Narrowing of the arteries is usually caused by atheroma (a build-up of fatty deposits in your blood vessels). See diagram 2.
What are the benefits of having a coronary angiogram?
This procedure will help your doctor to advise what further treatment will be best for you. If the narrowing is mild no further treatment may be needed. If it shows the narrowing is more severe your doctor may advise you to have a:
• Coronary angioplasty (a special balloon used to widen the artery).
• Stent (a short length of flexible tubing inserted to widen the vessel).
• Coronary artery bypass graft (a piece of vein used to bypass the narrowed section).
If you need to have any of these procedures:
• Your doctor or nurse will explain it to you in more detail.
• You will need to be referred to another hospital.
When your doctor has the results they will discuss these with you and, if needed, will explain the treatment choices available to help reduce your symptoms and improve your quality of life.
What are the risks and possible side effects?
Coronary angiogram is a safe procedure but does have some risks and possible complications. The risks must be compared to the benefits of having the procedure. The doctor who advised you to have this procedure will have considered these and decided this is the most appropriate test to help diagnose your condition. Your doctor or nurse will discuss your risks with you.
Steps will be taken to minimise (reduce) the chance of you developing these, for example, the procedure is carried out in a room, like an operating theatre, by an experienced doctor and you will be monitored (checked) throughout the procedure. Staff are trained to deal with these if needed.
Some side effects are common; usually these are minor and easy to treat. Serious complications are rare.
The risks and possible side effects include:
- Reaction to the dye (contrast medium). About 1 person in every 1,000 may have a minor reaction to the dye used during the procedure. This can cause mild nausea (feeling sick) or a minor skin rash. This usually settles on its own, but let your nurse or doctor know if this develops.
About 1 person in every 40,000 may have a more severe reaction. You will be monitored during and after the procedure and staff are ready to deal with any reaction, if needed. - Temporary renal dysfunction (your kidneys not working properly). About 5 people in every 100 may develop temporary renal dysfunction after this procedure.
You will not usually be aware if this happens and it should settle within 7 days of having the procedure, without needing any treatment. You are asked to drink a lot of water for a few days after the procedure to help reduce the chance of this happening.
This risk could be higher if you suffer from diabetes, existing renal problems, multiple myeloma (disease of the bone marrow) or are taking certain medications. - Problems with the circulation of blood which may cause you to have a fast, slow or an irregular heartbeat, a blockage in the artery in your arm or leg, a heart attack, stroke or death. This may affect about 1 patient in every 1,000. Your heart rate, rhythm and blood circulation will be monitored during and after the procedure.
This risk may be higher if you were to have an angina or heart attack during the procedure, or if you have diabetes. You will be monitored throughout the procedure and staff are trained to deal with these problems, if needed. - Damage to an artery. 1 person in every 500 may suffer damage to the artery as the catheter is inserted. Steps will be taken to treat this problem, if needed.
- Bleeding, bruising or infection after the procedure, especially at the catheter entry site. Any bleeding can be stopped by applying firm pressure over the wound site.
Some bruising may develop 1 to 2 days after the procedure but should then slowly settle over time. Steps are taken during the procedure to prevent an infection developing, for example, your skin will be cleaned and sterile instruments are used. - Radiation. The procedure uses ionising radiation (X-rays). Ionising radiation can cause cell damage that may, after many years or decades, turn cancerous.
The risk has been carefully compared to the benefit of having the procedure; the benefits of this examination outweigh any small radiation risk. The risk of this happening is low: it can happen to less than 1 patient in every 1,000 for this procedure.
For comparison the above radiation risk represents a very small increase over the natural risk of getting cancer of 1 person in every 2. It is the equivalent of 1 to 2 years natural radiation in the atmosphere.
If you think you may be pregnant you must let staff know as soon as possible before the examination. - Conscious light sedation (a drug which should make you feel comfortable and relaxed). This can occasionally cause problems with your breathing, heart rate and blood pressure. Careful monitoring by a fully trained healthcare professional will make sure they are identified and treated quickly.
What should I do before my coronary angiogram if I am not already in hospital?
You will be sent a letter telling you where and when to go for your procedure. You will be admitted to the Cardiology Day Unit (sometimes also called the Cath Lab) at the University Hospital of North Tees, as a day case patient.
You will be sent an appointment to attend a pre-assessment clinic 1 to 2 weeks before the date of your procedure. This is to check that you are well enough to have the procedure.
You will be seen by a nurse who will check your personal details, ask you questions about your health, perform an electrocardiogram – ECG (records (traces) the rhythm, rate and electrical activity of your heart), check your blood pressure and pulse. Your nurse may ask you to take some swabs to check if you have MRSA.
Please tell your nurse if you have:
- any allergies, for example, to medications (drugs) or seafood
- had reactions to medications
- had a coronary angiogram in the past.
They will explain the procedure, discuss the risks described earlier and answer any questions or concerns you may have. This is to make sure you understand everything before you sign the consent form.
You must arrange for a responsible adult to take you home and stay with you for at least the first 24 hours after your procedure as the effects of the sedation will affect your judgement or to call for help in case you develop any of the possible side effects.
If you have not made these arrangements you will not be able to be sedated and your coronary angiogram may have to be postponed.
If you take an anticoagulant, your pre-assessment nurse will tell you if you need to stop taking it before your procedure.
If you are a diabetic and take Metformin, you must stop taking it 2 days before and 2 days after your procedure.
You should continue to take all other medication as normal on the day of your procedure, including Aspirin or Clopidogrel (Plavix), unless you have been told not to.
You may have a light breakfast before 7.00am. You can continue to drink clear fluids, for example, water or diluted fruit squash.
Please if possible bring a dressing gown or comfortable clothing, slippers or shoes and if you wish, something to read before and after your procedure. If you need reading glasses please bring them with you.
Please do not bring any valuables into hospital with you.
You will not be able to drive after the procedure so you must arrange for a responsible adult to take you home and stay with you the night after your coronary angiogram. We do not advise you go home by bus.
Most people can return to work 2 days after the procedure but you may need to arrange a longer time off work if you do heavy manual work. Your doctor or nurse will advise you.
How long does the procedure take?
You will be admitted to the Cardiology Day Unit for the day. The procedure usually takes 20 to 60 minutes.
When your doctor has completed all the procedures planned for that session they will discuss the results of your procedure with you before you go home if you are an outpatient. This may mean you have to wait in the unit until late in the afternoon.
Your nurse will telephone the person you have arranged to collect you, when you are ready to go home.
If you are an inpatient you will be transferred back to the ward and will be told results by the doctor who is looking after you on the ward.
Who will be involved in my procedure?
A team of qualified and experienced healthcare professionals including a cardiologist (a doctor who specialises in conditions of the heart), nurse, cardiac physiologist (someone trained to perform and record special tests on the heart) and a radiographer (someone trained to take X-rays and scans) will be involved in your procedure.
However, qualified staff, who are learning this procedure, may also be involved. This would only be done under the supervision of qualified and experienced staff.
Can I be sedated for the examination?
Sedation can be given before and during the procedure, if needed or specially requested. This may be a light sedation given as a tablet about ½ hour before your procedure, to make you feel more relaxed.
On rare occasions stronger intravenous sedation and/or strong painkillers may be given just before or during the procedure if needed. This is called conscious sedation. You will still be awake but should feel more comfortable and relaxed.
What will happen when I arrive for my coronary angiogram as an outpatient?
A nurse will take you into the unit and check nothing has changed since your pre-assessment appointment. You will be shown to a screened area and asked to undress, put on a theatre gown and a dressing gown.
A nurse will check your blood pressure and pulse and insert a cannula (a fine tube) into a vein in your arm or the back of your hand using a small needle. This is in case you need to be given any medication during the procedure.
We operate a list system; this means you will be seen when it is your turn and not the time given for you to arrive at the unit.
A doctor or nurse will confirm your consent to having the procedure. When it is your turn you will be taken into the procedure room.
What will happen when I arrive for my coronary angiogram as an inpatient?
You will be taken to the Cardiology Day Unit when the unit is ready for you. The procedure usually takes 20 to 60 minutes but you may be in the Cardiology Day Unit for 3 to 4 hours before you are transferred back to your ward.
What will happen during the procedure?
A nurse will check your blood pressure and pulse and insert a cannula into a vein in your arm or the back of your hand using a small needle. This is in case you need to be given any medication during the procedure.
A doctor or nurse will confirm your consent to having the procedure. When it is your turn you will be taken into the procedure room.
Your heart rate will be monitored throughout the angiogram by placing sticky pads on your chest. These are attached to leads linked to an ECG machine to record your heart rate and rhythm.
A small plastic clip will be placed on one of your fingers or toes to check your pulse and the oxygen levels in your blood throughout the procedure. Do not worry, this does not hurt and is all routine.
You will be asked to lie on your back on a special trolley which has an X-ray machine above it. A nurse will be with you throughout the procedure to make sure you are comfortable.
A local anaesthetic is injected into your groin (top of your leg) or wrist to numb the area. When the area is numb your doctor will make a small incision (cut) in the skin above an artery. He or she will then pass a very fine, long, special catheter into the artery and up towards your heart.
You will not feel the catheter moving around in your chest but you may be aware of a missed or extra heart beat occasionally.
Contrast medium is then injected through the catheter into your coronary artery. The catheter may then be passed into the main pumping chamber of your heart, as this happens you may feel a warm flushing feeling and may feel you have wet yourself, even though you have not. This is normal and will wear off very quickly. You will be warned when to expect this.
X-rays are used to check the progress of the catheter as it is gently guided into the correct position. A number of X-rays are taken and recorded as a moving picture. This is called an angiogram. It shows your vessels filling with blood and whether there is any narrowing of any of the blood vessels.
This gives your doctor the vital information he or she needs to advise the best treatments for you, if needed.
Some people may have a short mild angina pain during the procedure. This does not mean anything is wrong, but you should tell your doctor if it happens.
When the procedure is over, the catheter is removed and the artery will be sealed using a ‘plug’ or pressure. The small wound does not usually need any stitches or dressing.
What happens after the procedure?
You will be taken back to the ward area for further monitoring.
You must not try to get off the trolley until your nurse says you can. You will be given a “nurse call buzzer” to use if you need anything.
If you have had your angiogram through the radial artery in your wrist you will be able to sit in a chair or walk around the unit. Your nurse will regularly check your blood pressure, pulses in your feet or wrist, and your wound site. You will be offered a drink and a snack.
When you have seen your doctor and are ready to be discharged the person you have arranged to take you home, will be asked to come and collect you.
When will I be told the results of my coronary angiogram?
Before you are discharged your doctor will discuss what he or she found during the procedure and discuss any further treatment choices, if needed. A letter will be sent to your GP giving details of the results.
How will I feel after the procedure?
The place where the catheter was inserted may feel a little tender for a few days. Most people get back to normal activities 1 to 2 days after the procedure.
How will I feel when I go home?
The place where the catheter was inserted may look bruised and feel a little tender or sore for a few days. Taking painkillers such as paracetamol should help. You should always follow the instructions provided in the leaflet supplied with your tablets.
What activities should I avoid when I go home?
The effect of sedation will stay with you for at least 24 hours so it is important you follow this advice.
There must be a responsible adult to take you home and look after you for the first 24 hours after your procedure as the effect of the sedation will affect your judgement. Your nurse will tell you how long you need to follow this advice.
For the first 12 hours you:
• must not go back to work.
• must not supervise children.
• must not make important decisions or sign any legal documents.
• must not operate machinery or electrical appliances.
• must not go near open flames or sources of high heat.
• must not take sleeping tablets.
• must not lock the toilet or bathroom door in case you need any help.
• should not smoke.
For the first 24 hours after your procedure you:
• must not drink alcohol because of the sedation and the contrast medium used.
For the first 48 hours after your procedure you:
• must not drive a car, ride a bicycle or motorcycle as this can cause bleeding. It is an offence to drive while unfit to do so because of the drugs used during sedation and it will probably invalidate your insurance.
Most people get back to normal activities 1 to 2 days after the procedure. You can eat and drink as normal. You should drink plenty of non-alcoholic fluids to help to flush the contrast medium out of your system.
When should I restart my medications?
If you take an anticoagulant and stopped taking it before your procedure your doctor or nurse will tell you when you should start taking it again and what dose to take.
If you are a diabetic and take Metformin you should start taking it again 2 days after your procedure.
You should continue to take any other medication as usual, unless your doctor or nurse tells you not to.
What should I do if my wound starts to bleed?
Depending upon the site used for your procedure, if there is any bleeding or oozing, you must:
• Press firmly over the wound in your wrist, or
• lie flat on a bed or floor and press firmly over the wound in your groin.
If this does not stop the bleeding and the bleeding is:
• Severe you must call 999 immediately.
• Not severe you should call your GP for advice.
You should contact your GP for advice if you develop:
• Any unusual pain.
• Any swelling, bruising or hard lumps in your groin or wrist.
- A temperature of 38°C (100.4°F) or higher.
When can I return to work?
This will depend on your job; most people can return to work 2 days after this procedure. If you do heavy manual work, or you drive a lot, you should not return to work for 4 to 5 days. Please ask your doctor or nurse for more advice.
Can I do heavy lifting?
You should take things easy and not do any heavy lifting for at least 3 days after your angiogram.
Can I have a bath or shower?
Yes, but do not have the water too hot for the first 24 hours.
When can I have sex again?
If you had your procedure performed through the femoral artery in your groin you should not have sex until at least 2 days after your angiogram.
Will I need a follow-up outpatient appointment?
Your doctor will tell you if he or she is going to arrange to see you again or if you are going to be referred to another hospital.
Contact numbers
If you need further advice, or have any problems, please contact:
University Hospital of North Tees
Cardiology Day Unit
Telephone: 01429 522020
Monday to Friday, 8.30am to 5.00pm
If no reply leave a message or telephone: 01429 522021
(These are Hartlepool codes but you will be diverted to North Tees.)
If the Cardiology Day Unit is closed and you have an urgent problem the night after your procedure you can contact:
Emergency Department
Telephone: 01642 382899
24 hours a day, 7 days a week
Further information is available from:
NHS Choices
Telephone: 111 (when it is less urgent than 999)
Calls to this number are free from landlines and mobile phones
or via the website at www.nhs.uk
Comments, concerns, compliments or complaints
Patient Experience Team (PET)
We are continually trying to improve the services we provide. We want to know what we’re doing well or if there’s anything which we can improve, that’s why the Patient Experience Team (PET) is here to help. Our Patient Experience Team is here to try to resolve your concerns as quickly as possible. The office is based on the ground floor at the University Hospital of North Tees if you wish to discuss concerns in person. If you would like to contact or request a copy of our PET leaflet, please contact:
Telephone: 01642 624719
Freephone: 0800 092 0084
Opening hours: Monday to Friday, 9:30am to 4:00pm
Email: [email protected]
Out of hours
Out of hours if you wish to speak to a senior member of Trust staff, please contact the hospital switchboard who will bleep the appropriate person.
Telephone: 01642 617617
Data protection and use of patient information
The Trust has developed Data Protection policies in accordance with Data Protection Legislation (UK General Data Protection Regulations and Data Protection Act 2018) and the Freedom of Information Act 2000. All of our staff respect these policies and confidentiality is adhered to at all times. If you require further information on how we process your information please see our Privacy Notices.
Telephone: 01642 383551
Email: [email protected]
Privacy NoticesLeaflet feedback
This leaflet has been produced in partnership with patients and carers. All patient leaflets are regularly reviewed, and any suggestions you have as to how it may be improved are extremely valuable. Please write to the Clinical Governance team, North Tees and Hartlepool NHS Foundation Trust, University Hospital of North Tees, TS19 8PE or:
Email: [email protected]
Leaflet reference: PIL
Date for Review: