Information for patients
This leaflet can be made available in other formats including large print, CD and Braille and in languages other than English, upon request.
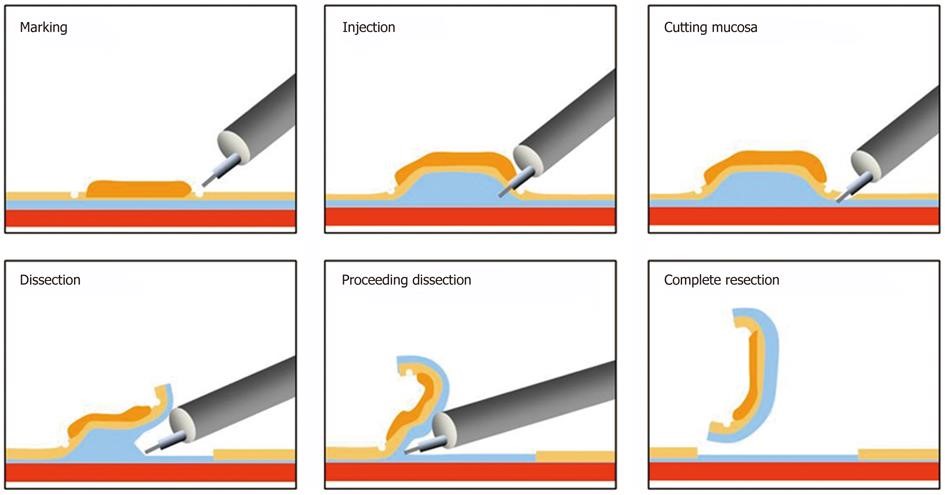
This leaflet will explain what Endoscopic Submucosal Dissection (ESD) is and when it is required. ESD involves removing concerning growths (polyps) from the wall of your gastrointestinal tract, including the stomach using an endoscope and an electrically heated knife.
Such growths in the stomach may be cancerous, potentially cancerous or harmless (benign).
Treatment usually involves removal of the growth, together with a small area of tissue around the growth.
This procedure is used for growths that are difficult or impossible to remove using other techniques.
The procedure follows advice from the National Institute for Health and Clinical Excellence (NICE), making the procedure as safe and efficient as possible.
What does the procedure involve?
- You will be under general anaesthetic.
- An endoscope (flexible camera) will be used to view your stomach wall and access the irregular area (polyp).
- Once the polyp has been located, fluid will be injected underneath it to lift the lesion away from the bowel wall muscle layers, making it easier and safer to remove.
- The polyp is then carefully resected from the bowel wall using a special diathermy (heat treated) knife.
What are the benefits of ESD?
Some polyps carry a risk of turning cancerous in the future. Not all polyps will make this progression, and if they do it usually takes several years to happen. Some larger polyps can already contain early cancer cells.
The main benefit of this procedure is to avoid you having to undergo major surgery. Removal of the polyp in one piece allows us to examine it in detail under a microscope, giving the best opportunity to know if it has been fully removed. Removing the polyp in one piece also reduces the chance of it growing back in the future. [1, 2]
What care will I need after the procedure?
ESD is planned as a one-day procedure. This means that if all goes well, and depending on the time of your appointment, you may go home after the anaesthetic has worn off.
You will be asked to look for symptoms such as blood in your stools (poo) or dark/black-coloured poo and any fever or pain for 2 to 3 weeks after the procedure. If you do get these symptoms, you should return to hospital for examination.
How will I feel after the procedure?
Due to the anaesthetic drugs, you have been given, you may feel sleepy for a few hours following the procedure.
For a few days after the procedure, you may experience:
- Mild discomfort (soreness)
- Indigestion and nausea
- Minor bleeding
This is a normal part of your healing process and may vary depending on the area that had to be removed during the procedure.
What if something goes wrong?
If you experience any of the symptoms described (blood, fever, severe pain), we may need to keep you in hospital as an inpatient. This usually involves close observation of your vital signs, sometimes a repeat camera examination (e.g. to stop bleeding) and occasionally open surgery to repair your stomach in case of a puncture (“perforation”).
How well does the procedure work?
Studies show that growth removal rates, where the growth was removed in 1 piece, were higher for lesions treated with ESD than with endoscopic mucosal resection (EMR).
Research shows that ESD achieves single piece resection in 8-9 out of 10 cases, with clear margins (“cure”) achieved in approximately 7 out of 10 cases1.
What are the risks and potential complications involved?
The main risks of ESD are: [1, 2]
- Bleeding during or after the procedure, in about 5-10% of patients. This is generally able to be stopped during the procedure but severe bleeding may require a hospital stay and involve a blood transfusion.If you take any drugs to thin your blood, you will be asked to stop these temporarily prior to ESD. If you usually take Warfarin, we may arrange for you to have daily injections of heparin instead. This will help to reduce the risk of bleeding. Most patients do not develop problems while they are not taking their blood thinning medication, however there is an increased risk of developing blood clots or having a stroke during this time. This is something you may wish to discuss with the endoscopist prior to your procedure.
- Perforation (puncture) in the stomach in up to 3% of patients. Usually, a puncture can be treated through the scope, but may involve a stay in hospital.
- Very rarely, an emergency operation may be required to surgically repair the site of perforation or treat severe bleeding if endoscopic treatment is not possible. The operation may be “open” or “key-hole (laparoscopic)” surgery.
- Any emergency operation may be life threatening (lead to death) or alter your future quality of life.
Research suggests both perforation and serious bleeding rates are not common following the ESD procedure. However, these risks are slightly higher compared to Endoscopic Mucosal Resection EMR.
Other risks include:
Rarely, causing a cancerous lesion to spread (potentially becoming incurable)
Extra surgery or treatment with chemotherapy or radiotherapy may be needed after ESD, if analysis under the microscope suggests deep cancerous invasion of the stomach wall.
There is a chance that due to complications, the growth may not be able to be removed in one piece.
There is also a chance that regrowth (recurrence) may occur months after the procedure, in up to 5% of patients (1, 2).
Are there alternative procedures to ESD?
Yes, the main alternative procedures include:
Endoscopic Mucosal Resection or EMR
This procedure often removes growths in more than one piece, making it difficult to analyse under a microscope. It is often uncertain as to whether the polyp has been completely removed. Follow up checks are often needed to ensure regrowth doesn’t occur. Risks of EMR are similar to ESD (bleeding and perforation) although the likelihood of such a complication occurring is lower than with ESD.
Laparoscopic or open surgery
This procedure requires general anaesthesia and aims to remove all or part of the stomach, depending on the nature, location, and size of the growth. This is generally associated with longer recovery and may carry greater risks.
Do nothing.
There is also the option of doing nothing and leaving the polyp in your stomach untreated. The risks of this option are that the polyp will continue to grow and develop into cancer in the future (if not already cancer). There is also a risk of the polyp causing symptoms if left untreated. This decision must be carefully considered after discussion with your consultant.
What does this mean for me?
Your doctor or nurse specialist will explain the procedure in full detail as well as the risks and benefits involved. You will be given the opportunity to ask any further questions.
References
- Pimentel-Nunes P, Libânio D, Bastiaansen BAJ et al. Endoscopic submucosal dissection for superficial gastrointestinal lesions: European Society of Gastrointestinal Endoscopy (ESGE) Guideline – Update 2022. Endoscopy 2022; 54: 591-622. doi:10.1055/a-1811-7025
2. NICE. Endoscopic submucosal dissection of gastric lesions. 2010.
Further information is also available from the National Institute of Health and Clinical Excellence website: https://www.nice.org.uk/guidance/IPG335
Comments, concerns, compliments or complaints
Patient Experience Team (PET)
We are continually trying to improve the services we provide. We want to know what we’re doing well or if there’s anything which we can improve, that’s why the Patient Experience Team (PET) is here to help. Our Patient Experience Team is here to try to resolve your concerns as quickly as possible. The office is based on the ground floor at the University Hospital of North Tees if you wish to discuss concerns in person. If you would like to contact or request a copy of our PET leaflet, please contact:
Telephone: 01642 624719
Freephone: 0800 092 0084
Opening hours: Monday to Friday, 9:30am to 4:00pm
Email: [email protected]
Out of hours
Out of hours if you wish to speak to a senior member of Trust staff, please contact the hospital switchboard who will bleep the appropriate person.
Telephone: 01642 617617
Data protection and use of patient information
The Trust has developed Data Protection policies in accordance with Data Protection Legislation (UK General Data Protection Regulations and Data Protection Act 2018) and the Freedom of Information Act 2000. All of our staff respect these policies and confidentiality is adhered to at all times. If you require further information on how we process your information please see our Privacy Notices.
Telephone: 01642 383551
Email: [email protected]
Privacy NoticesLeaflet feedback
This leaflet has been produced in partnership with patients and carers. All patient leaflets are regularly reviewed, and any suggestions you have as to how it may be improved are extremely valuable. Please write to the Clinical Governance team, North Tees and Hartlepool NHS Foundation Trust, University Hospital of North Tees, TS19 8PE or:
Email: [email protected]
Leaflet reference: PIL1469