Information for patients
This leaflet can be made available in other formats including large print, CD and Braille and in languages other than English, upon request.
Your doctor has advised you to have a chest drain inserted.
This leaflet tells you about insertion of a chest drain and will help you to understand what will happen during and after the procedure.
What is a chest drain?
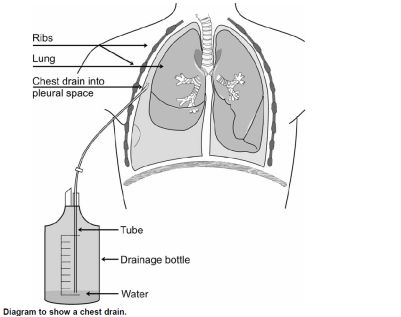
A chest drain is a small, flexible, sterile tube (usually as thin as, or thinner than a pen) which is inserted into the chest cavity in the space between the inside of the chest wall and the edge of the lung.
A local anaesthetic will be injected into the skin and tissue to numb the area around where your chest drain needs to be inserted.
Your doctor will then make a small incision (cut) and will insert the drain so it enters the pleural cavity (space between your chest wall and your lung).
This will allow fluid, air, pus or blood to drain away (see diagram below). The tube does not go into your lung.
Why do I need a chest drain?
The most common reasons for insertion of a chest drain can include:
- A pneumothorax (collection of air between the lung and the chest wall).
- A pleural effusion (build up of fluid between the lung and the chest wall).
- An empyema (build up of infected fluid or pus between the lung and the chest wall).
- A haemopneumothorax (build-up of blood and air between the lung and the chest wall).
Your doctor will explain the reason you need a chest drain. If you have any questions or are unsure about anything, please ask your doctor.
Who will insert my chest drain?
A qualified doctor will insert your chest drain. This is usually a junior hospital doctor who has been trained to insert a chest drain.
However, you may be asked if a junior doctor, who is learning this procedure, may insert your drain. This would only be done under the supervision of a more experienced doctor.
If you do not agree to this, it will not affect your treatment in any way.
What will happen when my chest drain is inserted?
Chest drains are usually inserted on a ward or in the Emergency Department.
A doctor will explain the reasons why you need a chest drain and discuss the risks and possible complications before asking you to consent to the procedure. If you have any questions or are unsure about anything, please ask your doctor.
Normally a chest drain is inserted in the side of your chest while you sit back against some pillows, with your arm lifted up over your head.
Sometimes the chest drain might be inserted towards the back of your chest when you will be asked to sit forwards, resting on a bedside table.
When you are comfortable the skin around the area will be cleaned. Your doctor will inject a local anaesthetic to numb your skin, muscle, ribs and the lining around the inside of your chest wall.
They will then make a small incision in your skin and carefully insert the chest drain. The chest drain will be kept in place by a suture (stitch) and a dressing will be put over the area.
As the fluid or air around your lungs drains you should be able to breathe more easily. You may feel some slight discomfort as your lung expands again.
After your chest drain is inserted the tube will be connected to a special bottle containing sterile water. An underwater seal prevents air moving back up the tube.
Your nurses will keep checking the bottle and record any drainage. The team will also send you for a Chest X-ray.
Will it be painful?
Local anaesthetic is injected into your skin before the procedure begins so you should not feel any pain, but you may feel some pressure or pushing.
You must tell your doctor or nurse if it becomes painful as extra local anaesthetic or other painkilling drugs can be given, if needed.
How can I help look after my chest drain?
Once the chest drain has been inserted it is important you take care of it. The chest drain will be fixed using a suture but extra care should be taken when turning over, getting into or out of bed, or a chair.
It is important the drainage bottle is kept below the level of your chest drain at all times so that fluid does not go back up the tube.
What will happen if the tube becomes blocked?
Sometimes the tube can become blocked. If this happens you may suddenly become short of breath or develop a swelling on your chest wall due to air in the tissues (surgical emphysema).
If you think this may have happened, you must tell one of your nurses immediately.
How long will I need the chest drain?
This will vary from patient to patient. You may need it for 1 day, many days; or even longer, depending on your condition. Your doctor may arrange for you to have a number of chest X-rays during this time to check your progress.
Sometimes when a chest drain has been in for a few days a senior respiratory doctor may ask for some suction to be attached to your chest drain to help settle your problem more quickly.
What happens when my chest drain is removed?
When your doctor decides your chest drain can be removed a nurse or doctor will remove the dressings and gently remove the drain.
You will be asked to either hold your breath or breathe out as the chest drain is being removed. This helps to prevent air being sucked back into your chest.
The stitch may be removed or left in place for a few more days to help the wound to heal.
If, after having your drain removed, you develop:
- Increased pain
- Difficulty breathing
- A temperature higher than 38°C (100.4°F)
You must tell one of your doctors or nurses immediately.
If you have any other worries or concerns, please tell one of your doctors or nurses.
What are the risks and possible complications?
Insertion of a chest drain is a very safe procedure but does have some risks and possible complications. These will be discussed with you at the time you consent to the procedure.
The most common risks and possible complications include:
Discomfort or pain during the procedure
You will be given a local anaesthetic to numb the area before the procedure begins. Please tell your doctor if you feel more than slight discomfort.
Chest drain becoming dislodged (moved)
The drain can sometimes become dislodged from the pleural cavity even though it is secured in place. This can happen when turning over or getting into or out of bed.
Please take care when moving about. If your chest drain becomes dislodged it may have to be re-inserted.
The chest drain not being placed in the pleural cavity
Usually this is because the tube has not been inserted far enough and still remains in the tissues around the chest wall.
Sometimes this is only found after a chest X-ray has been taken. If this happens your doctor will need to insert the drain further into your chest, or insert a new tube.
Infection
The risk of this happening is reduced by cleaning your skin before the chest drain is inserted and using single use, sterile equipment and chest drain. If an infection develops it will be treated with antibiotics.
Surgical emphysema (air getting into the skin and soft tissues around the chest drain).
This is more likely to happen in patients who are having a drain inserted because of pneumothorax. It can also develop if the tube becomes blocked. Treatment may involve the insertion of another, sometimes slightly wider, drain.
Other, much rarer complications can include:
Penetration (puncture) of major organs including the lung, stomach, spleen, heart or large blood vessels leading to or from the heart.
Doctors take great care to minimise (reduce) the risk of this happening and it is very rare.
Vasovagal attack (slowing of the heart rate and a fall in blood pressure which could cause you to faint). This can sometimes happen while your chest drain is being inserted if you are afraid, in pain or shock.
Staff are trained to deal with all of the risks and complications. Should complications develop steps will be taken to treat these.
Staff are trained to deal with all of the risks and complications. Should complications develop steps will be taken to treat these.
Contact numbers
If you have any worries or concerns, you should contact the immediate nurses or doctors looking after you In addition you may contact the respiratory team below:
North Tees and Hartlepool NHS Foundation Trust
Department of Respiratory Medicine
Telephone: 01642 624936
Monday – Friday, 9.00am to 5.00pm
Lung Health
Telephone: 01642 624270
Monday – Friday, 9.00am to 5.00pm
Further information is available from:
NHS Choices
Telephone: 111 (when it is less urgent that 999)
Calls to this number are free from landlines and mobile phones
or via the website at www.nhs.uk
Asthma and Lung UK
Telephone: 03000 030 555
Monday – Friday, 9.00am to 5.00pm
or via the website at: https://www.asthmaandlung.org.uk/
Information used in the development of this leaflet
National Patient Safety Agency (NPSA), Risks of chest drain insertion, May 2008, NPSA/2008/RRR03.
British Thoracic Society (BTS) Guidelines for the management of pleural disease, updated July 2023;
https://www.brit-thoracic.org.uk/document-library/guidelines/pleural-disease/bts-guideline-for-pleural-disease/
Comments, concerns, compliments or complaints
Patient Experience Team (PET)
We are continually trying to improve the services we provide. We want to know what we’re doing well or if there’s anything which we can improve, that’s why the Patient Experience Team (PET) is here to help. Our Patient Experience Team is here to try to resolve your concerns as quickly as possible. The office is based on the ground floor at the University Hospital of North Tees if you wish to discuss concerns in person. If you would like to contact or request a copy of our PET leaflet, please contact:
Telephone: 01642 624719
Freephone: 0800 092 0084
Opening hours: Monday to Friday, 9:30am to 4:00pm
Email: [email protected]
Out of hours
Out of hours if you wish to speak to a senior member of Trust staff, please contact the hospital switchboard who will bleep the appropriate person.
Telephone: 01642 617617
Data protection and use of patient information
The Trust has developed Data Protection policies in accordance with Data Protection Legislation (UK General Data Protection Regulations and Data Protection Act 2018) and the Freedom of Information Act 2000. All of our staff respect these policies and confidentiality is adhered to at all times. If you require further information on how we process your information please see our Privacy Notices.
Telephone: 01642 383551
Email: [email protected]
Privacy NoticesLeaflet feedback
This leaflet has been produced in partnership with patients and carers. All patient leaflets are regularly reviewed, and any suggestions you have as to how it may be improved are extremely valuable. Please write to the Clinical Governance team, North Tees and Hartlepool NHS Foundation Trust, University Hospital of North Tees, TS19 8PE or:
Email: [email protected]
Leaflet reference: PIL1127
Date for Review: August 2026